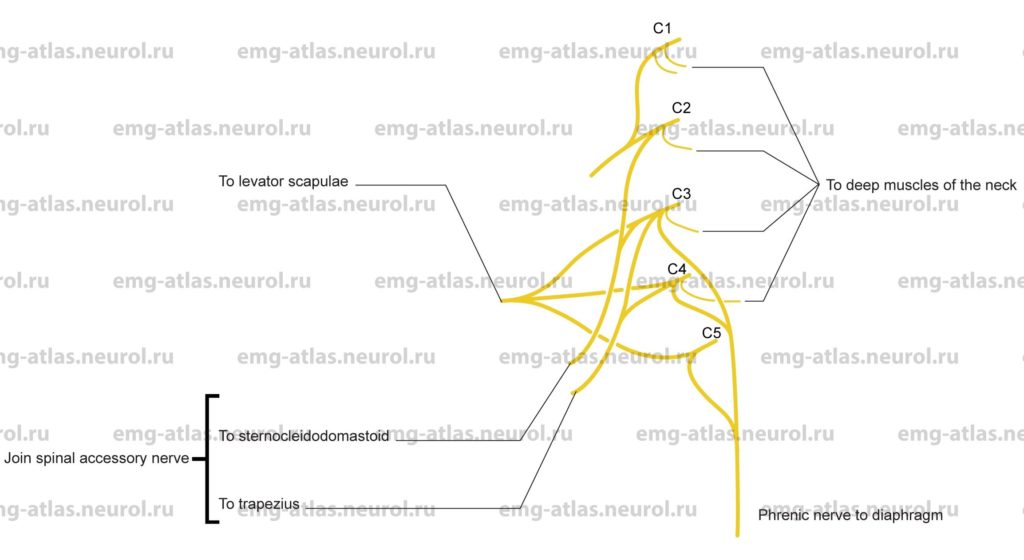
Diagram of the major muscular branches of the cervical plexus (lateral view).
The cervical plexus is formed by the upper four cervical ventral rami (Gray’s Anatomy, 1977). It lies deep to the sternocleidomastoid muscle and anterior to the scalenus medius and levator scapulae muscles. Its branches can be divided into two groups, superficial and deep. The superficial branches provide cutaneous innervation to the head, neck, and chest and include the lesser occipital, great auricular, transverse cervical, and supraclavicular nerves. The deep branches are largely muscular branches distributed to deep muscles of the neck, including the anterior recti and rectus capitis lateralis muscles and the scalenus medius. These branches also supply the sternocleidomastoid, trapezius, levator scapulae, and the diaphragm.
The diaphragm receives its motor supply solely from the cervical plexus via the phrenic nerve, which arises from the third, fourth, and fifth cervical nerves. The muscular branches from the cervical plexus to the stemocleidomastoid and trapezius communicate with the spinal accessory nerve, which provides most of the innervation to these muscles. Cervical branches to the stemocleidomastoid are derived chiefly from the second and third cervical nerves, while branches to the trapezius are derived from the third and fourth cervical nerves. Branches to the levator scapulae are derived from the third and fourth cervical nerves, which are joined by the fifth cervical nerve via the dorsal scapular nerve of the brachial plexus.
Anatomical Illustrations
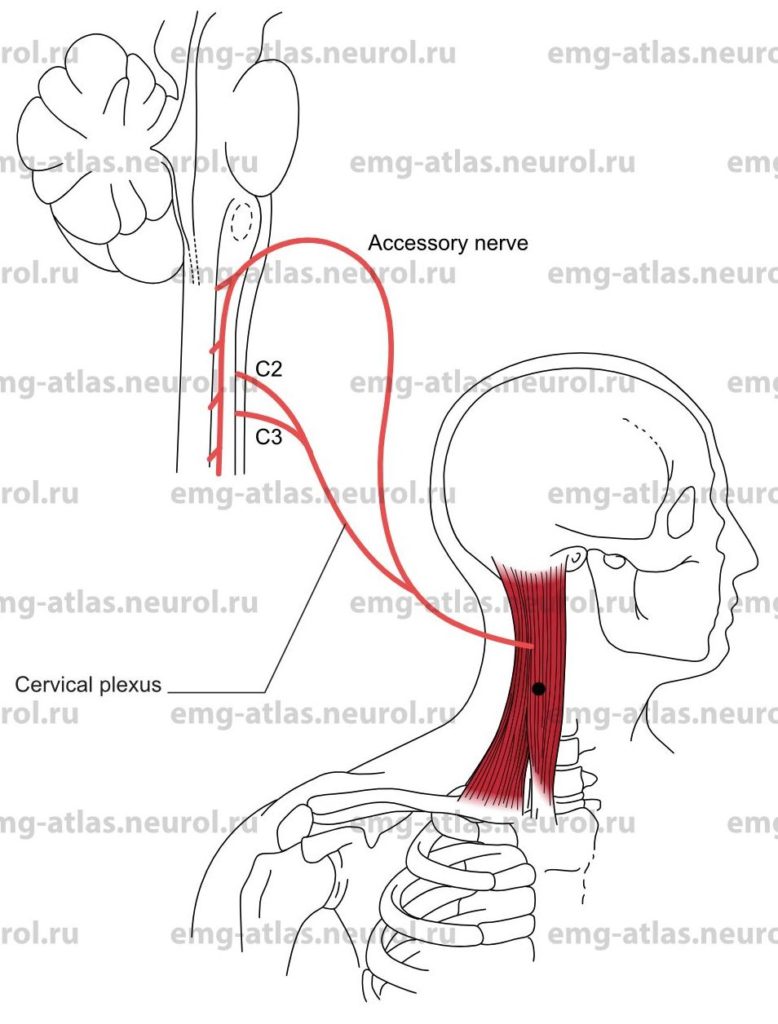
Sternocleidomastoid
Innervation
Innervation is via the spinal accessory nerve and branches from the C2, C3, and sometimes the C4 cervical spinal nerves (Gray’s Anatomy, 1995).
Origin
The sternal head arises from the upper part of the manubrium sterni.
The clavicular head arises from the medial third of the clavicle.
Insertion
Insertion is at the lateral surface of the mastoid process.
Activation Maneuver
Rotation of the head (opposite to the muscle studied) activates the muscle.
EMG Needle Insertion
Insert the needle at the midpoint between the mastoid process and the sternal origin. Enter the muscle obliquely, and direct the needle parallel to the muscle fibers.
Pitfalls
If the needle is inserted too medially and anteriorly, it may penetrate the common, internal, or external carotid arteries.
Clinical Comments
Needle examination may show neurogenic changes when injury to the spinal accessory nerve or branches from C2, C3, and C4 produces axonal loss. Note: The spinal accessory nerve may be damaged during lymph node dissection in the posterior triangle of the neck, sparing the Sternocleidomastoid but affecting the trapezius (Donner and Kline, 1993).
Cervical dystonia (torticollis) often begins with tonic or clonic spasms of the Sternocleidomastoid muscle.
Anatomical Illustrations
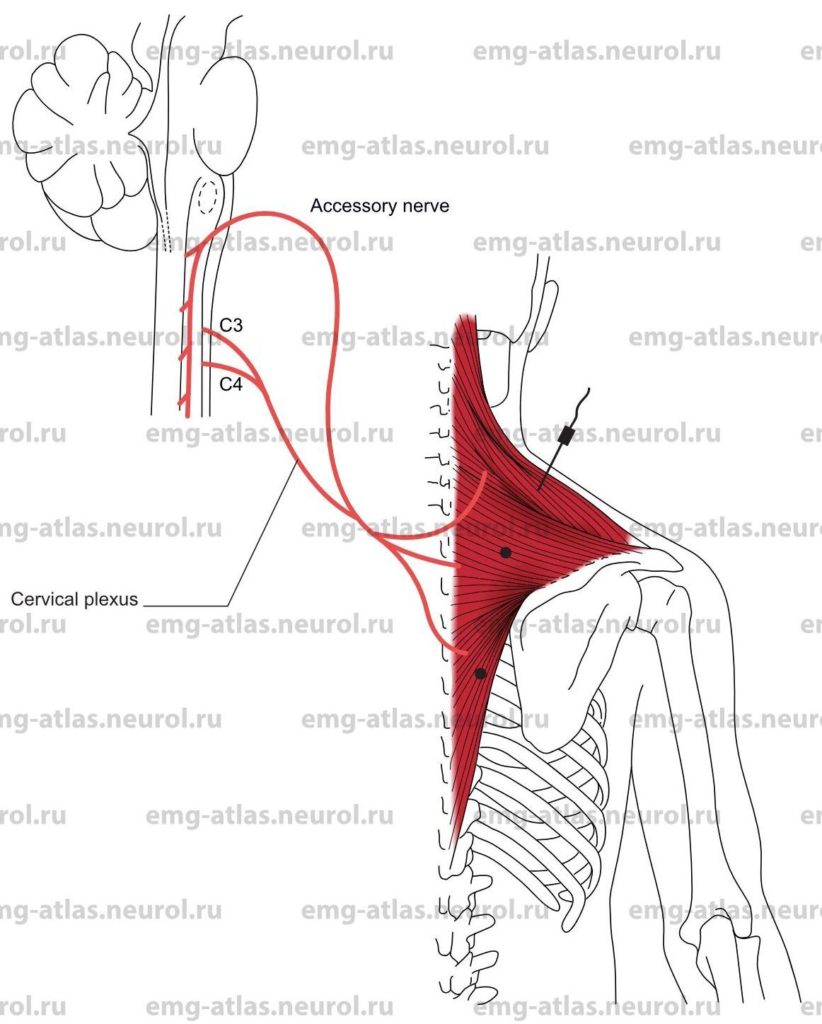
Trapezius
Innervation
Innervation is via the spinal accessory nerve and branches from the C3 and C4 cervical spinal nerves (Gray’s Anatomy, 1995).
Origin
The upper fibers originate at the occipital bone and ligamentum nuchae.
The middle fibers originate at the spinous processes of the seventh cervical and upper thoracic vertebrae.
The lower fiber originate at the spinous processes of the lower thoracic vertebrae.
Insertion
Upper fibers: Insertion is at the outer third of posterior border of clavicle.
Middle fibers: Insertion is at the acromion process and the crest of the spine of the scapula.
Lower fibers: Insertion is at the medial surface of the spine of the scapula.
Activation Maneuver
Upper fibers: Shrug or elevate the shoulder.
Middle fibers: Retract the scapula.
Lower fibers: Rotate the scapula by elevating the arm. EMG Needle Insertion
Upper fibers: Insert the needle at the angle of the neck and shoulder.
Middle fibers: Insert the needle midway between the spine of the scapula and the spinous processes at the same level.
Lower fibers: Insert the needle 3–4 cm lateral to the spinous processes of the lower thoracic vertebrae.
Pitfalls
Upper fibers: If the needle is inserted too deeply, it may be in the levator scapulae (supplied by the dorsal scapular nerve and C3, C4) or other neck muscles.
Middle fibers: If the needle is inserted too deeply, it may be in the rhomboideus major or minor, which are supplied by the dorsal scapular nerve.
Lower fibers: If the needle is inserted too deeply and caudally, it may be in the latissimus dorsi, which is supplied by the thoracodorsal nerve.
Clinical Comments
Needle examination may show neurogenic changes when injury to the spinal accessory nerve or branches from C3 and C4 produces axonal loss.
The most common etiology of spinal accessory mononeuropathy is iatrogenic injury related to biopsy of cervical lymph nodes in the posterior triangle of the neck or benign tumor removal (Berry et al., 1991; Donner and Kline, 1993). This type of injury affects the trapezius but spares the sternocleidomastoid.
Anatomical Illustrations
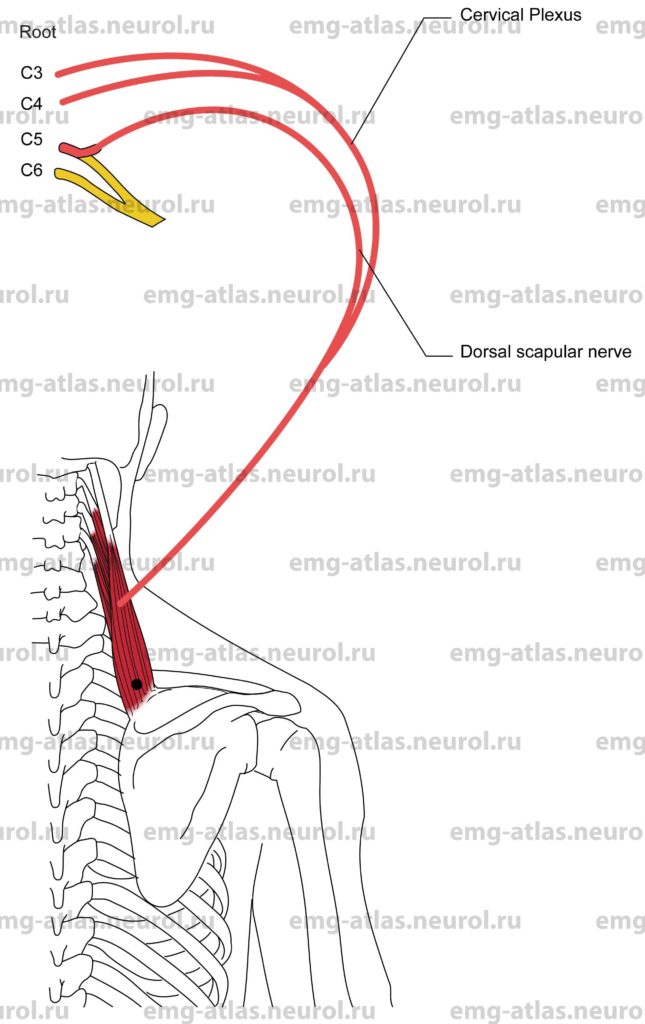
Levator Scapulae
Innervation
Innervation is via the anterior rami of C3, C4, and C5 and the latter branch via the dorsal scapular nerve.
Origin
The levator scapulae originate at the transverse processes of the upper four cervical vertebrae.
Insertion
Insertion is at the posteromedial border of the scapula, between the superior angle and the spine of the scapula.
Activation Maneuver
Elevation of the scapula (which assists the trapezius in the shrugging shoulders) activates the levator scapulae.
EMG Needle Insertion
Insert the needle along the superiomedial margin of the scapula.
Pitfalls
If the needle is inserted too superficially, it will be in the trapezius muscle, which is supplied by the spinal accessory nerve.
If the needle is inserted too deeply, it may be in the paraspinal muscles.
Clinical Comments
Neurogenic changes in this muscle on needle examination usually indicate C3-C5 radiculopathy.
Look for neurogenic changes in other C5-innervated muscles to confirm C5 radiculopathy.