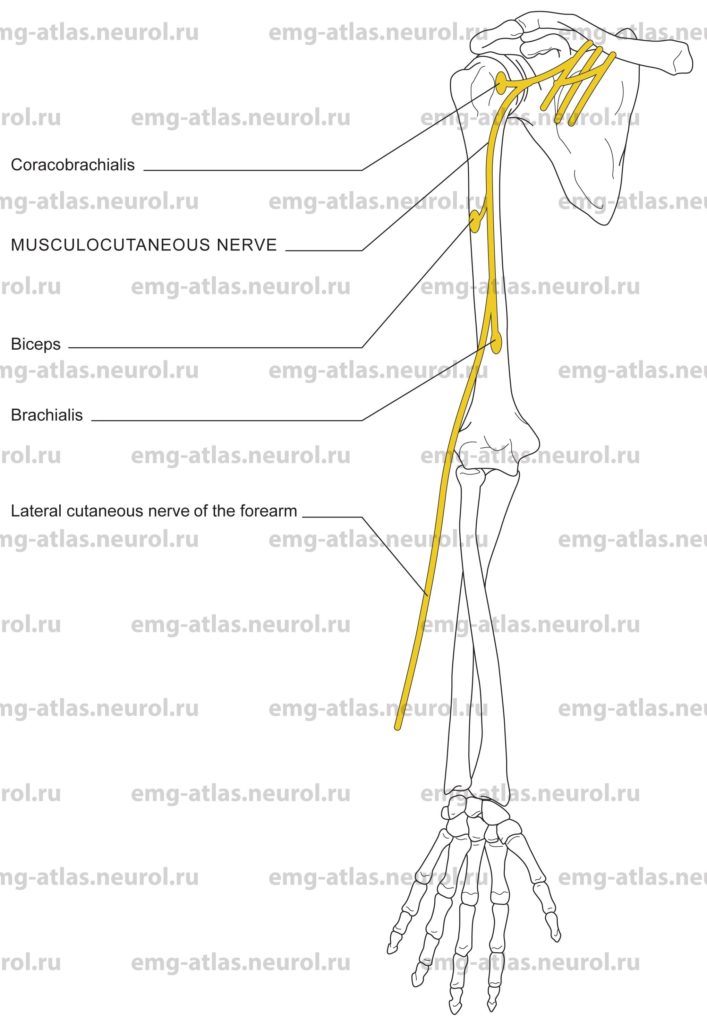
Diagram of the musculocutaneous nerve and the muscles that it supplies.
Fibers to the musculocutaneous nerve are derived primarily from the fifth and sixth cervical roots, with an occasional contribution from the seventh cervical root (Gray’s Anatomy, 1995). The nerve trunk arises from the lateral cord of the brachial plexus near the lower border of the pectoralis minor muscle. It proceeds downward to pierce the coracobrachialis muscle, which it innervates. The nerve passes through this muscle to reach the interval between the brachialis and biceps muscles. The nerve supplies both of these muscles as it descends between them, just below the elbow it pierces the deep fascia lateral to the tendon of the biceps, continuing as the lateral cutaneous nerve of the forearm. This branch provides cutaneous innervation to the lateral aspect of the forearm, as far as the midline anteriorly and posteriorly, and as distal as the base of the thenar eminence and dorsolateral aspect of the wrist (Sunderland, 1968).
Musculocutaneous Nerve Lesion
Etiology
Trauma and deep penetrating wounds can cause a musculocutaneous lesion.
Neuralgic amyotrophy (idiopathic brachial plexopathy) can be causative.
Rarely, entrapment of the musculocutaneous nerve as it passes through the coracobrachialis (Braddom and Wolfe, 1978) can cause a musculocutaneous lesion.
General Comments
Trauma almost always results in combined lesions of the musculocutaneous nerve and the lateral cord of the brachial plexus (Sunderland, 1968).
Clinical Features
Wasting and weakness of the coracobrachialis, biceps, and brachialis can occur. In complete lesions of the musculocutaneous nerve, the supinator and brachioradialis hypertrophy and may compensate for the loss of the biceps and brachialis muscles.
Loss of the biceps tendon reflex occurs.
There is sensory loss over the lateral aspect of the forearm.
Electrodiagnostic Strategy
Demonstrate neurogenic EMG changes in the coracobrachialis, biceps, and brachialis.
EMG of other C5 and C6 muscles may be necessary to exclude cervical radiculopathy.
Musculocutaneous motor conduction studies may show reduced amplitude or absence on the affected side.
Sensory conduction studies of the lateral cutaneous nerve of the forearm may show reduced amplitude or absence on the affected side.
Anatomical Illustrations
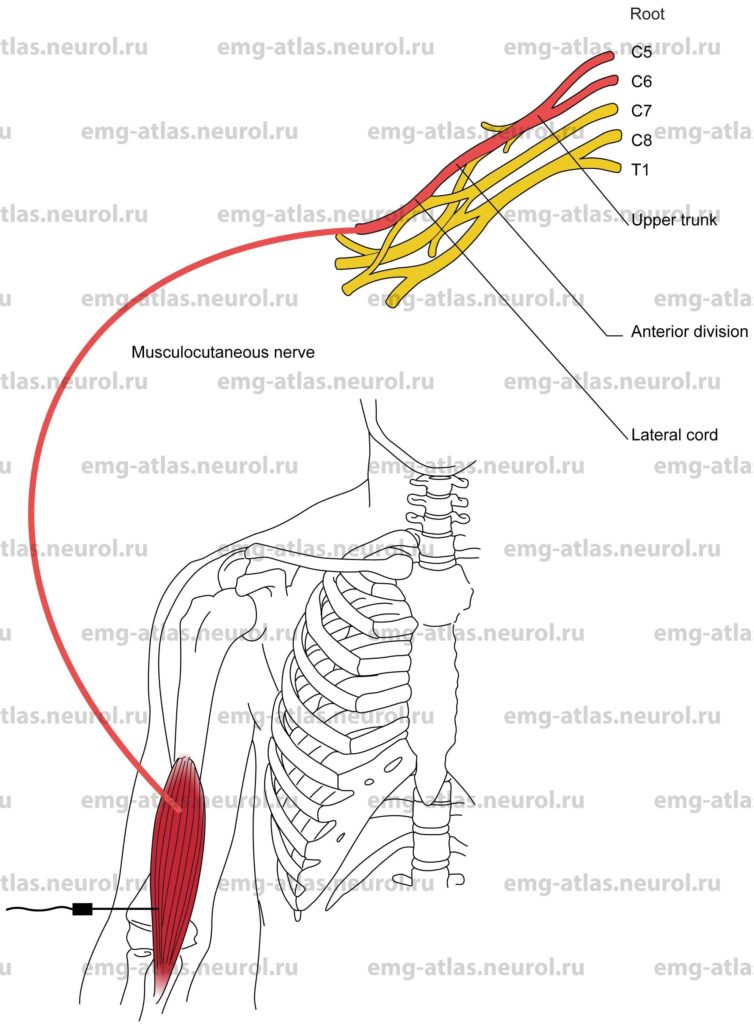
Brachialis
Innervation
Innervation is via the musculocutaneous nerve, lateral cord, upper trunk, and roots C5, C6. Note: A small lateral portion of the muscle may receive radial nerve innervation (C7 root).
Origin
The brachialis originates in the lower half of the anterior surface of the humerus.
Insertion
Insertion is at the ulnar tuberosity and the anterior part of the coronoid process of the ulna.
Activation Maneuver
Flexion of the forearm at the elbow activates the muscle. EMG Needle Insertion
Lateral approach: Insert the needle 4–5 cm proximal to the elbow crease just lateral to and under the biceps.
Medial approach: This approach is not recommended because it risks injury to the median nerve, brachial artery, and basilic vein.
Pitfalls
If the needle is inserted too distally and posteriorly, it may be in the proximal brachioradialis or extensor carpi radialis longus; these muscles are supplied by the radial nerve.
If the needle is inserted too proximal and posteriorly, it may be in the lateral head of the triceps, which is supplied by the radial nerve.
Clinical Comments
Needle examination may show neurogenic changes when injury to the musculocutaneous nerve produces axonal loss.
In brachial plexopathy, needle examination may show neurogenic changes when lateral cord pathology has resulted in axonal loss.
In Cs, C6 radiculopathy, needle examination may show neurogenic changes when root pathology has resulted in axonal loss (i.e., in moderate to severe radiculopathy).
In Erb’s palsy (C5, C6 root avulsion), needle examination will show neurogenic changes.
Anatomical Illustrations
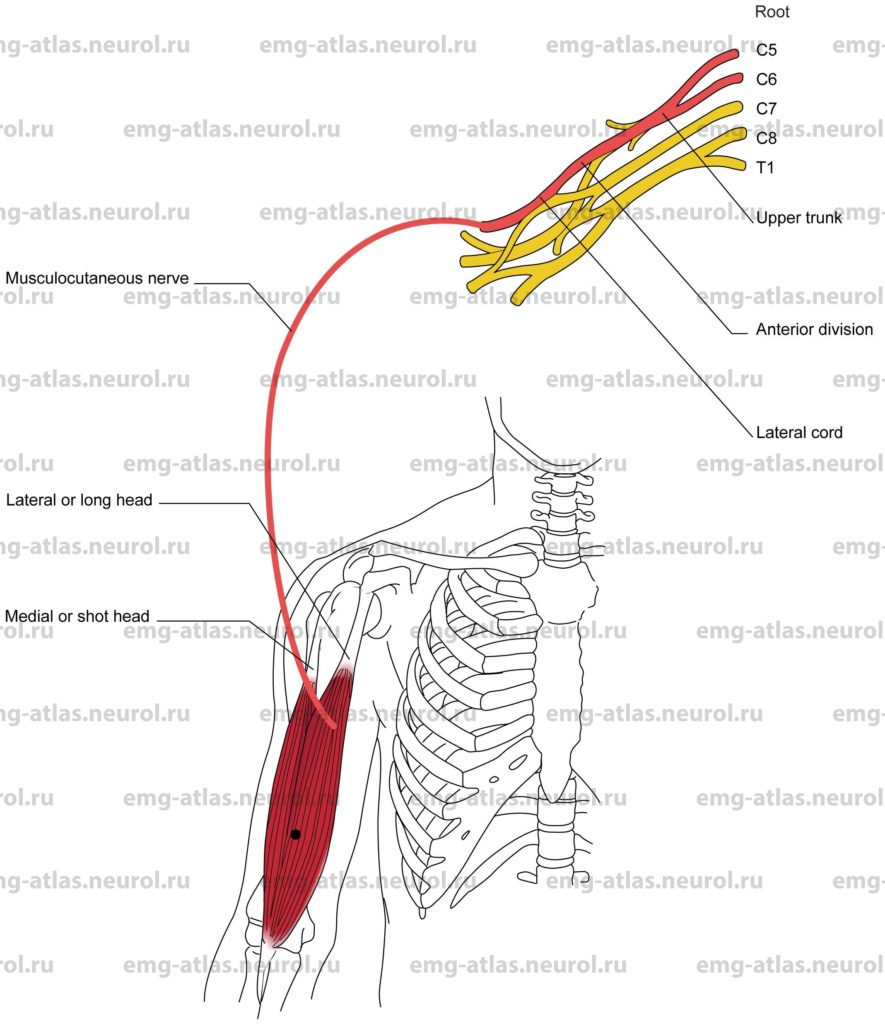
Biceps Brachii
Innervation
Innervation is via the musculocutaneous nerve, lateral cord, upper trunk, and roots C5, C6.
Origin
The medial or short head of the biceps brachii originates at the coracoid process of the scapula.
The lateral or long head originates at the supraglenoid tubercle of the scapula.
The humeral head, which is found in 10% of cases, arises from the humerus at the insertion of the coracobrachialis.
Insertion
Insertion is at the posterior aspect of the radial tuberosity (the tuberosity lies distal to the medial part of the neck of the radius).
Activation Maneuver
Flexion and supination of the forearm at the elbow activates the biceps brachii. To a slight extent, the biceps also acts to flex the arm at the shoulder. EMG Needle Insertion
Insert the needle into the midarm anteriorly, into bulk of the muscle.
Pitfalls
If the needle is inserted too proximally, it may be in the anterior deltoid (supplied by the axillary nerve) or the pectoralis major (supplied by the medial and lateral pectoral nerves).
If the needle is inserted too deeply, it may be in the brachialis, which is also supplied by the musculocutaneous nerve.
Clinical comments
Needle examination may show neurogenic changes when injury to the musculocutaneous nerve produces axonal loss.
In brachial plexopathy, needle examination may show neurogenic changes when lateral cord pathology has resulted in axonal loss.
In C5, C6 radiculopathy, needle examination may show neurogenic changes when root pathology has resulted in axonal loss (i.e., in moderate to severe radiculopathy).
In Erb’s palsy (C5, C6 root avulsion), needle examination will show neurogenic changes.
Anatomical Illustrations
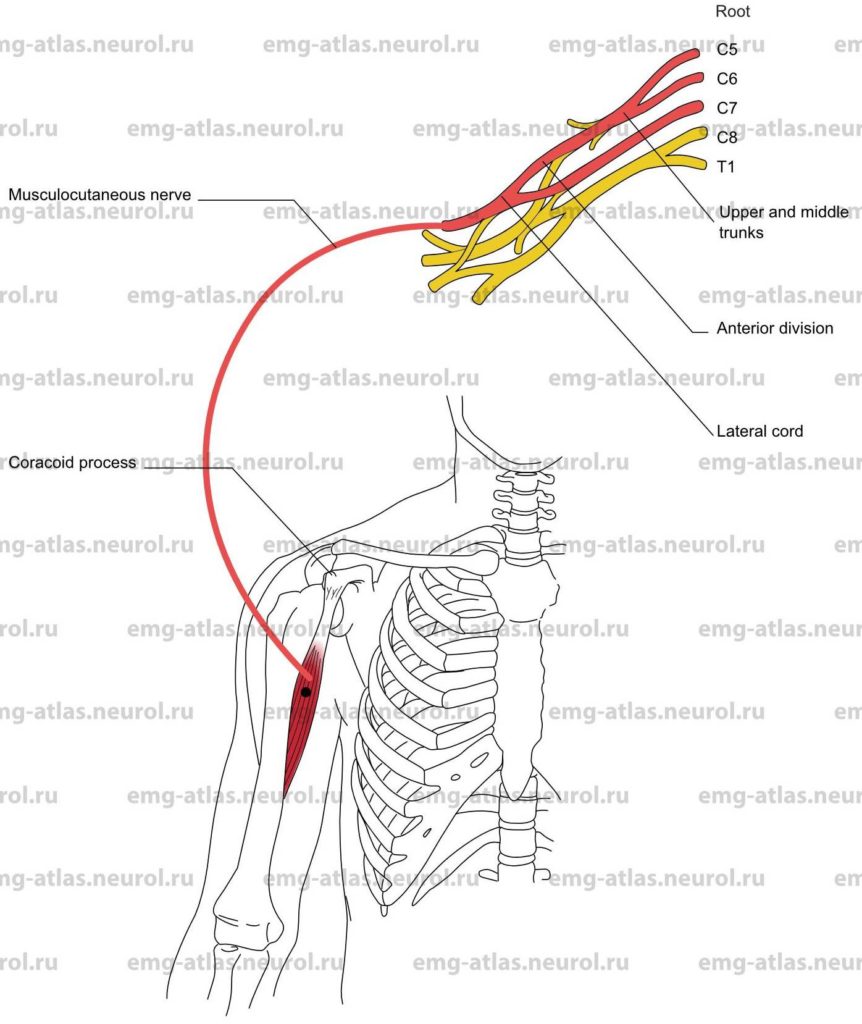
Coracobrachialis
Innervation
Innervation is via the musculocutaneous nerve, lateral cord, upper and middle trunks, and roots C5, C6, C7.
Origin
The coracobrachialis originates at the apex of the coracoid process of the scapula.
Insertion
Insertion is at the medial surface of the shaft of the humerus.
Activation Maneuver
Forward elevation of the humerus activates the muscle. The coracobrachialis stabilizes the head of the humerus in relation to the glenoid fossa of the scapula. EMG Needle Insertion
Insert the needle 6-8 cm distal to the coracoid process along the volar aspect of the arm.
Pitfalls
If the needle is inserted too laterally and superficially, it may be in the short head of the biceps, which is also innervated by the musculocutaneous nerve.
If the needle is inserted too proximal and superficial, it may be in the anterior deltoid, which is supplied by the axillary nerve.
Clinical Comments
Needle examination may show neurogenic changes when injury to the musculocutaneous nerve produces axonal loss.
In brachial plexopathy, needle examination may show neurogenic changes when lateral cord pathology has resulted in axonal loss.
In C5, C6, C7 radiculopathy, needle examination may show neurogenic changes when root pathology has resulted in axonal loss (i.e., in moderate to severe radiculopathy).