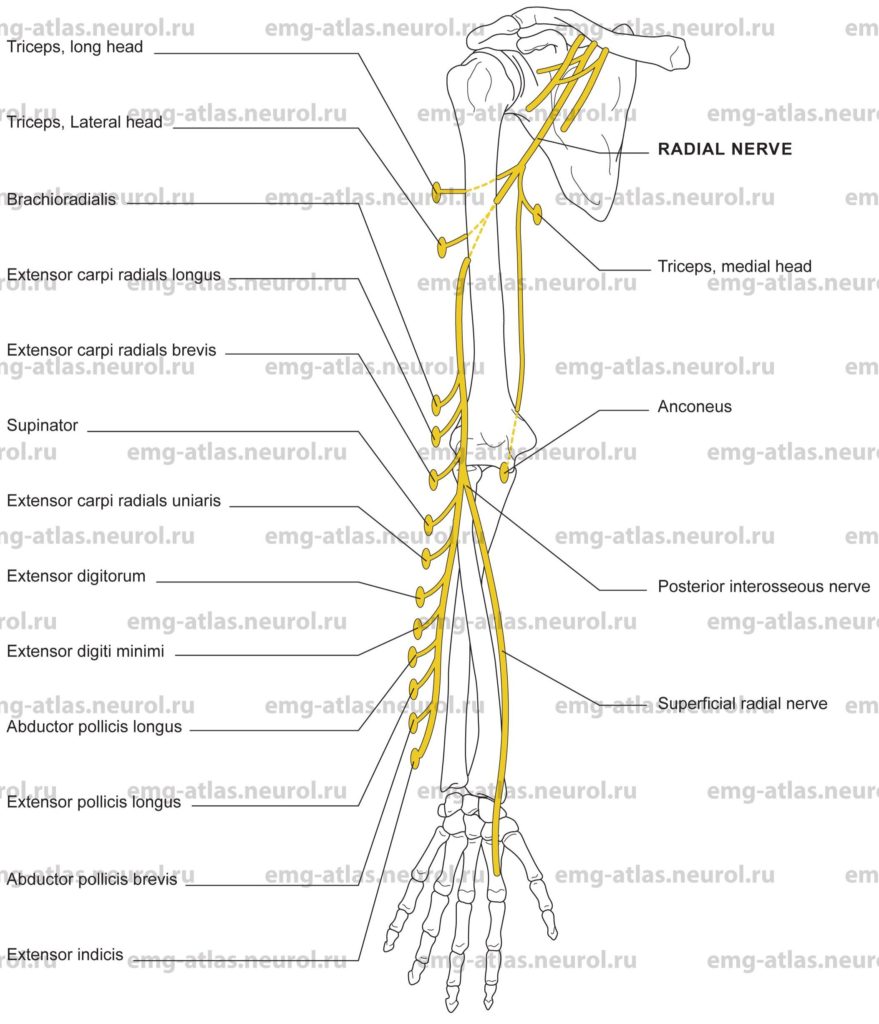
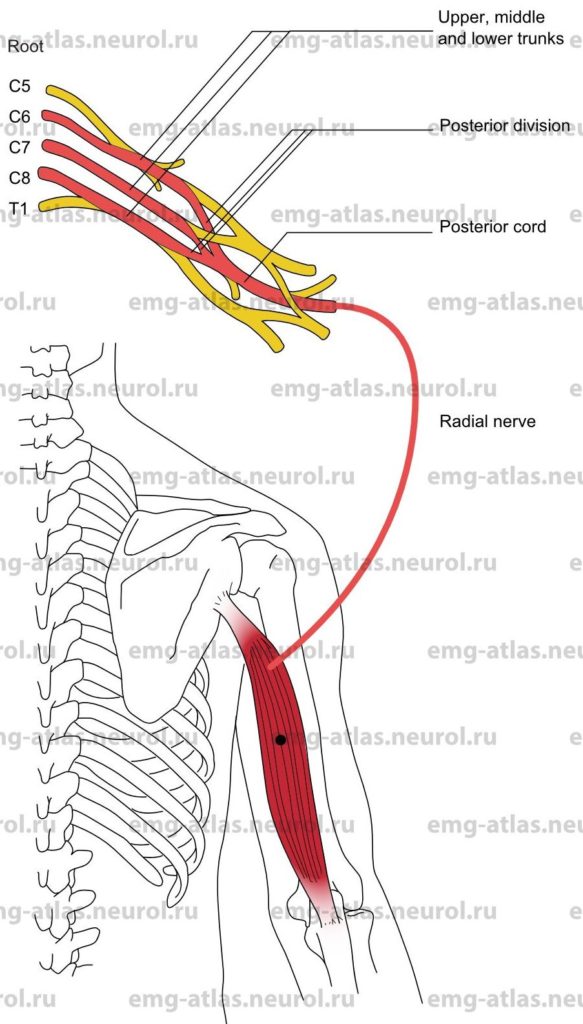
Diagram of the radial nerve and the muscles that it supplies.
The radial nerve is the largest branch of the brachial plexus, arising from the posterior cord and the fifth, sixth, seventh, and eighth cervical roots, with occasional contribution from the first thoracic root (Gray’s Anatomy, 1995). From its origin on the posterior axillary wall, it descends behind the axillary artery to reach the angle between the medial aspect of the arm and the posterior wall of the axilla (brachio-axillary angle). Branches to the heads of the triceps and anconeus arise in the axilla and brachio-axillary angle.
With the profunda brachii artery, the radial nerve inclines downward between the long and medial heads of the triceps, after which it passes obliquely along the back of the humerus in the spiral groove (also known as the radial groove). Here it is in direct contact with bone. On reaching the lateral side of the humerus, the nerve pierces the lateral intermuscular septum to enter the anterior compartment. It then descends in the furrow between the brachialis medially and brachioradialis laterally. The nerve gives off branches to the brachialis (this muscle is supplied primarily by the musculocutaneous nerve) and brachioradialis. The nerve is overlapped, in turn, by the extensor carpi radialis longus and extensor carpi radialis brevis. The radial nerve supplies both muscles, although the extensor carpi radialis brevis may receive its nerve supply from the superficial radial or posterior interosseous nerve (Sunderland, 1968).
Anterior to the lateral epicondyle, the radial nerve divides into its two terminal branches: the posterior interosseous nerve and the superficial radial nerve. The former is a pure muscular nerve that innervates the supinator before passing through the arcade formed by the superficial and deep heads of this muscle (arcade of Frohse). On the dorsum of the forearm, the posterior interosseous nerve divides in a variable manner to innervate the extensor carpi ulnaris, extensor digitorum communis, extensor digit! minimi, abductor pollicis longus, extensor pollicis longus and brevis, and extensor indicis. The superficial radial branch is primarily a sensory nerve. It provides cutaneous innervation to the dorsum of the hand lateral to the ring finger, dorsum of the thumb, radial aspect of the thenar eminence, and dorsum of the index, middle, and radial half of the ring fingers as far distally as the middle phalanx.
Although the radial nerve, or its branches, may be involved in penetrating injuries at any level, there are certain sites where the nerve is more prone to injury (Sunderland, 1968). In the brachio-axillary angle, compression may result from a misused crutch or from fractures of the upper third of the humerus. In the region of the spiral groove and lateral intermuscular septum, compression neuropathies of the radial nerve are common and widely recognized. The nerve is most commonly damaged by fractures of the humerus or during deep intoxication with the arm draped over the edge of a bed, chair, or bench (Saturday night palsy). In its course through the supinator (arcade of Frohse), the posterior interosseous nerve is prone to damage from fractures of the upper third of the radius and less commonly from entrapment. Injury to the superficial radial branch may result from tight (handcuffs handcuff neuropathy) or carelessly administered intravenous infusions.
Radial Nerve Lesion in the Arm
Etiology
Compression of the nerve in the spiral groove (radial groove) of the humerus can cause a radial nerve lesion in the arm.
The condition is called «Saturday night palsy» when sedatives or alcohol produces deep sleep in someone and an arm is draped over the edge of a bed, chair, or bench.
The condition is called «honeymooner’s palsy» when compression results from the weight of a partner’s head lying on the arm.
A radial nerve lesion can occur secondary to a fracture of the humerus, prolonged or excessive muscle contraction (as in masons, carpenters, or athletes in throwing sports), anatomical anomalies of the triceps, and deep intramuscular injections.
General Comments
A radial nerve lesion in the arm is a common compression neuropathy.
Predisposing factors include diabetes, malnutrition, alcohol or sedative use, and hereditary susceptibility to pressure palsies (Brown and Watson, 1993).
The differential diagnosis includes lead poisoning, porphyria, diabetes, and periarteritis nodosa.
Clinical Features
Wrist drop occurs with a radial nerve lesion in the arm.
There is normal function of the triceps (extension of forearm at elbow).
There is weakness of the brachioradialis and all other muscles supplied by the radial nerve beyond the spiral groove.
Pain is not a typical feature, but it may be perceived in the area of the lateral epicondyle, radial styloid, or dorsum of hand.
Numbness can occur in the distribution of the superficial radial nerve and occasionally in the territory of the posterior cutaneous nerve of the forearm.
Most cases of «Saturday night palsy» fully resolve in days to a few weeks, which is consistent primarily with a demyelinating lesion. Delayed or incomplete recovery implies a greater degree of axonal loss.
Electrodiagnostic Strategy
Use electrodiagnostic evaluation to confirm a focal lesion (conduction block, slowing of conduction velocity) at the spiral groove and to obtain information on severity and prognosis. Cases characterized by conduction block resolve quickly; those with axonal loss and wallerian degeneration show a reduction of motor or sensory amplitudes and resolve slowly or incompletely.
In cases of axonal loss, EMG may show neurogenic changes (spontaneous activity, abnormal motor unit potentials, and abnormal recruitment) in the brachioradialis and in all other muscles supplied by the radial nerve distal to the spiral groove.
EMG is normal in cases of demyelination and in the early stages of axonal loss in which wallerian degeneration has not yet occurred.
EMG of the triceps is normal.
The superficial radial sensory response is reduced in amplitude or absent in cases of axonal loss (normal in cases of demyelination and in the early stages of axonal loss).
EMG of nonradial innervated C7 muscles may be necessary to exclude C7 radiculopathy.
Radial Nerve Lesion in the Axilla
Etiology
Compression of the nerve in the axilla by high-riding crutches can cause the condition called crutch neuropathy.
A radial nerve lesion can occur secondary to shoulder trauma, humerus fractures, tumor, or anatomical anomalies of the coracobrachialis or triceps.
Clinical Features
Wrist drop occurs with a radial nerve lesion in the axilla.
Weakness occurs in all muscles supplied by the radial nerve, including the triceps.
The triceps reflex is absent
Numbness occurs in the distribution of the superficial radial nerve and occasionally in the the territory of the posterior cutaneous nerve of the forearm.
Most cases fully resolve in days to a few weeks, which is consistent primarily with a demyelinating lesion. Delayed or incomplete recovery implies a greater degree of axonal loss.
Electrodiagnostic Strategy
Use electrodiagnostic evaluation to obtain evaluation to obtain information on severity and prognosis. Cases associated with axonal loss and wallerian degeneration show a reduction of motor or sensory amplitudes and resolve slowly or incompletely.
In cases of axonal loss, EMG may show neurogenic changes in the triceps and all other muscles supplied by the radial nerve.
EMG is normal in cases of demyelination and in the early stages of axonal loss in which wallerian degeneration has not yet occurred.
The superficial radial sensory response is reduced in amplitude or absent in cases of axonal loss (normal in cases of demyelination and in the early stages of axonal loss).
EMG of nonradial innervated C7 muscles may be necessary to exclude C7 radiculopathy.
Posterior Interosseous Nerve Syndrome
Etiology
Compression of the nerve as it passes between the two layers of the supinator muscle in the arcade of Frohse can cause posterior interosseous nerve syndrome.
Posterior interosseous nerve syndrome can occur secondary to radial subluxation, a fracture of the proximal radius, prolonged or repeated pronation-supination movements, tumors (lipoma), neuralgic amyotrophy, and compression by the extensor carpi radialis brevis.
General Comments
Posterior interosseous nerve syndrome is also known as the supinator syndrome.
Injury to the posterior interosseous nerve is usually associated with trauma (fractures, gunshot wounds, lacerations) ratherthan with true entrapment.
Clinical Features
There is normal supination of the forearm and radial wrist extension (supinator and extensor carpi radialis are normal).
Weakness occurs in the extensor carpi ulnaris; attempted wrist extension results in characteristic radial deviation of the wrist.
Weakness occurs during finger extension and thumb extension. Thumb abduction may be normal because the abductor pollicis brevis (median nerve) is unaffected.
There is pain in the lateral upper forearm (usually 5-8 cm distal to the lateral epicondyle).
There is no sensory impairment because the superficial radial nerve arises above the arcade of Frohse.
Electrodiagnostic Strategy
The superficial radial sensory response is normal.
Motor studies may reveal a focal lesion (conduction block, slowing of conduction velocity) across the entrapment (Kimura, 1989). Cases characterized by conduction block resolve quickly; those associated with wallerian degeneration show a reduction of motor amplitude and resolve slowly or incompletely.
EMG may show neurogenic changes (spontaneous activity, abnormal motor unit potentials, and abnormal recruitment) in all muscles supplied by the posterior interosseous nerve below the supinator.
EMG of radial innervated muscles (triceps, anconeus, brachioradialis, and extensor carpi radialis longus and brevis) is normal.
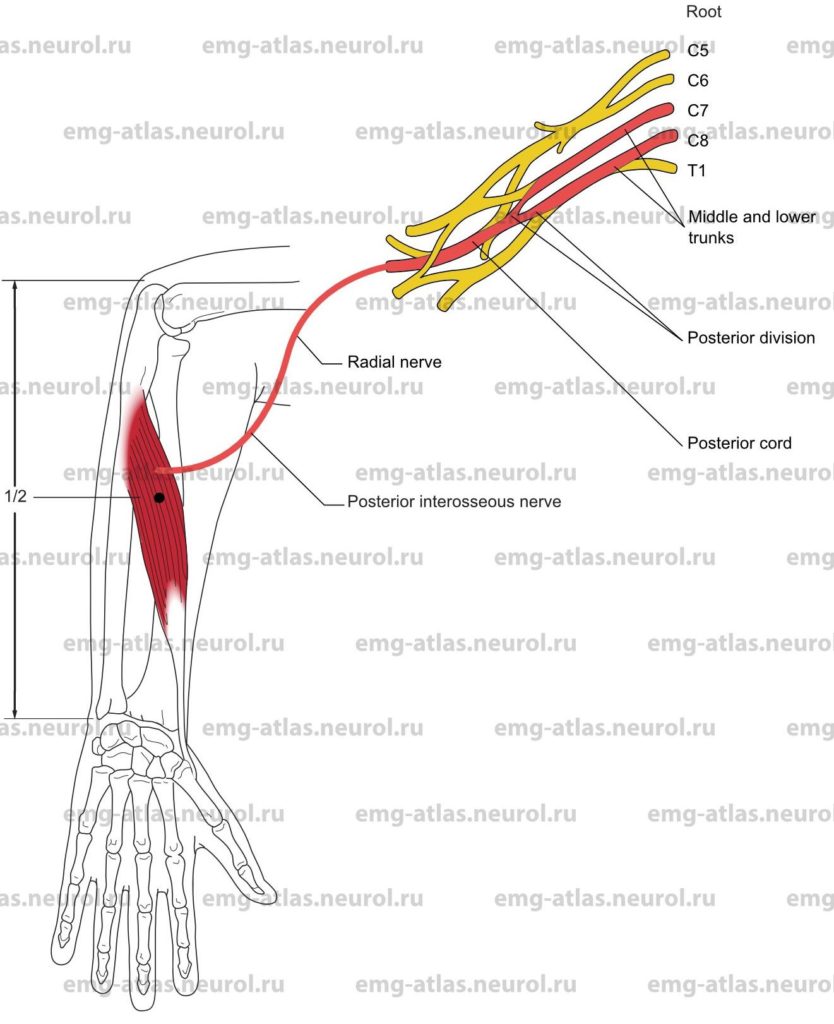
Anatomical Illustrations
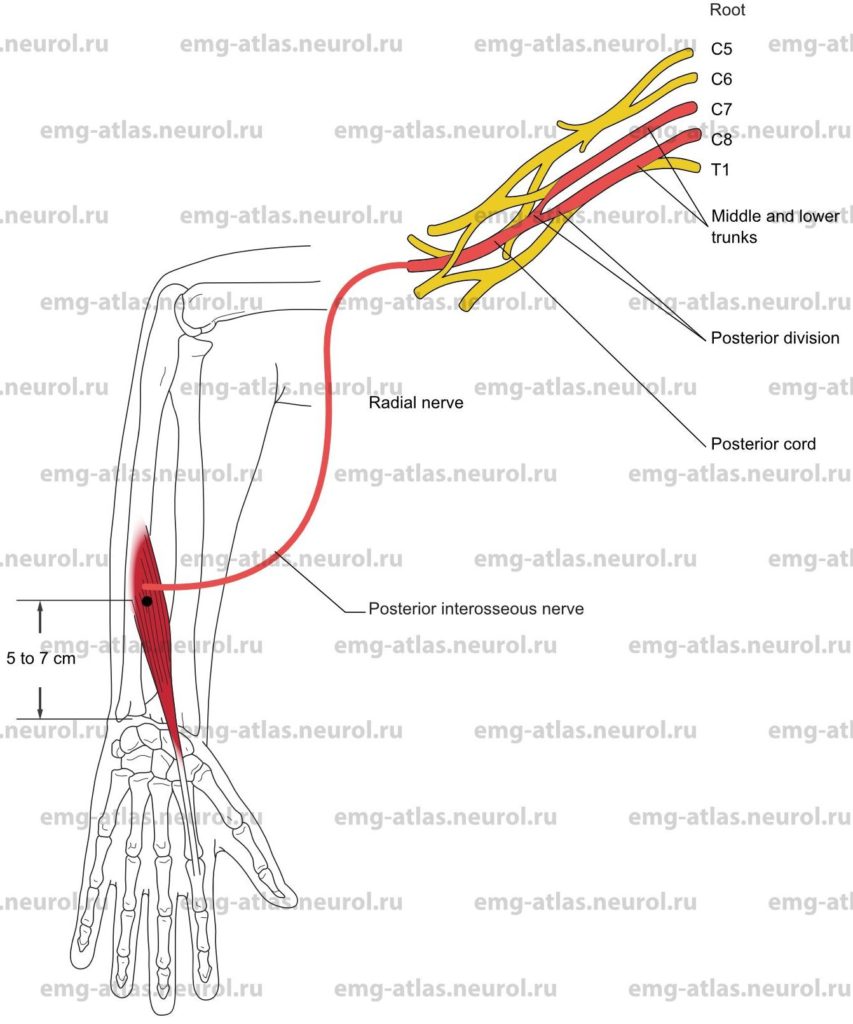
Extensor Indicis
Innervation
Innervation is via the posterior interosseous nerve, radial nerve, posterior cord, middle and lower trunks, and roots C7, C8.
Origin
The extensor indicis originates at the posterior surface of the lower half of the shaft of the ulna and adjacent interosseous membrane.
Insertion
The extensor indicis joins the tendon of the extensor digitorum communis to the index finger.
Activation Maneuver
Extension of the index finger activates the muscle. EMG Needle Insertion
Insert the needle 5-7 cm proximal to the ulnar styloid just radial to the shaft of the ulna. Hint: Follow the tendon proximally to where it intersects the ulna.
Pitfalls
If the needle is inserted too laterally (radially), it may be in the extensor pollicis longus, which also receives innervation from the posterior interosseous nerve.
Clinical Comments
The extensor indicis is usually the most distal muscle innervated by the posterior interosseous branch of the radial nerve.
In a radial nerve lesion at the axilla (crutch neuropathy), needle examination may show neurogenic changes when compression produces axonal loss.
In a radial nerve lesion at the upper arm (Saturday night palsy), needle examination may show neurogenic changes when compression at the spiral groove produces axonal loss.
In a posterior interosseous nerve lesion, needle examination may show neurogenic changes when pathology produces axonal loss.
Anatomical Illustrations
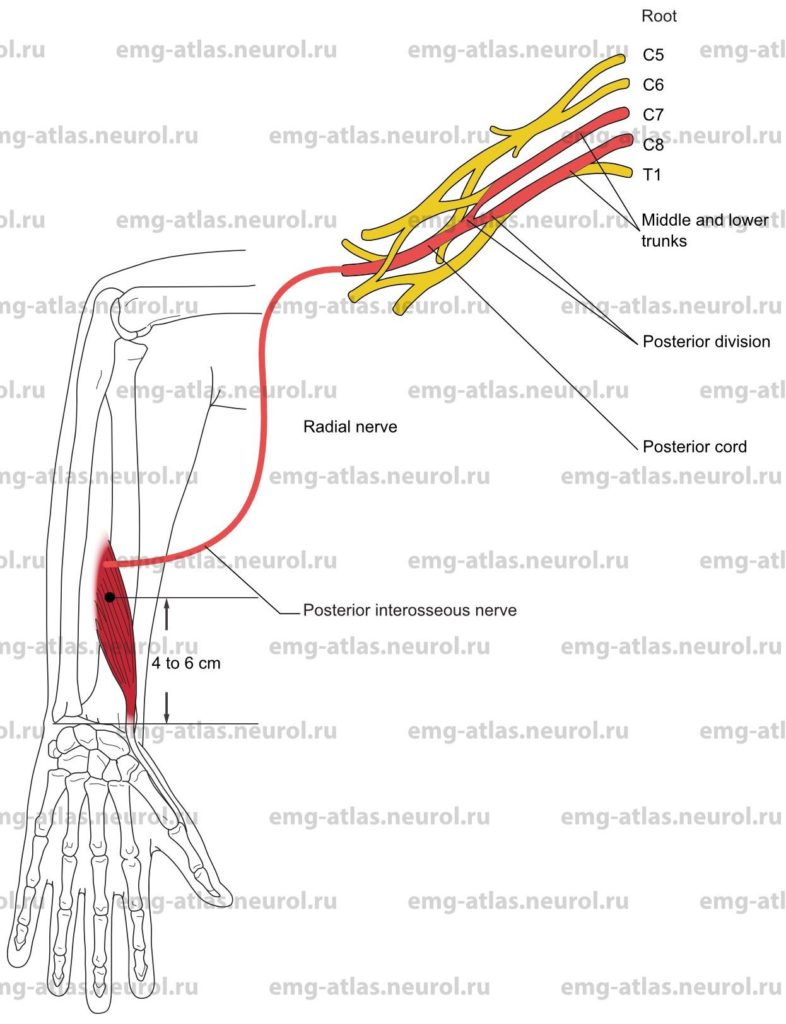
Extensor Pollicis Brevis
Innervation
Innervation is via the posterior interosseous nerve, radial nerve, posterior cord, middle and lower trunks, and roots C7, C8.
Origin
The extensor pollicis brevis originates at the posterior surface of the shaft of the radius, below the origin of the abductor pollicis longus, and adjacent interosseous membrane.
Insertion
Insertion is at the base of the first phalanx of the thumb. (Note: The tendon passes through the same groove as the abductor pollicis longus tendon on the outer side of the styloid process, forming the radial border of the anatomical «snuffbox»)
Activation Maneuver
Extension of the proximal phalanx of the thumb activates the muscle.
EMG Needle Insertion
Insert the needle 4-6 cm proximal to the wrist over the ulnar aspect of the radius.
Pitfalls
If the needle is inserted too proximally, it may be in the abductor pollicis longus, which also receives innervation from the posterior interosseous nerve.
Clinical Comments
In a radial nerve lesion at the axilla (crutch neuropathy), needle examination may show neurogenic changes when compression produces axonal loss.
In a radial nerve lesion at the upper arm (Saturday night palsy), needle examination may show neurogenic changes when compression at the spiral groove produces axonal loss.
In a posterior interosseous nerve lesion, needle examination may show neurogenic changes when pathology produces axonal loss.
Anatomical Illustrations
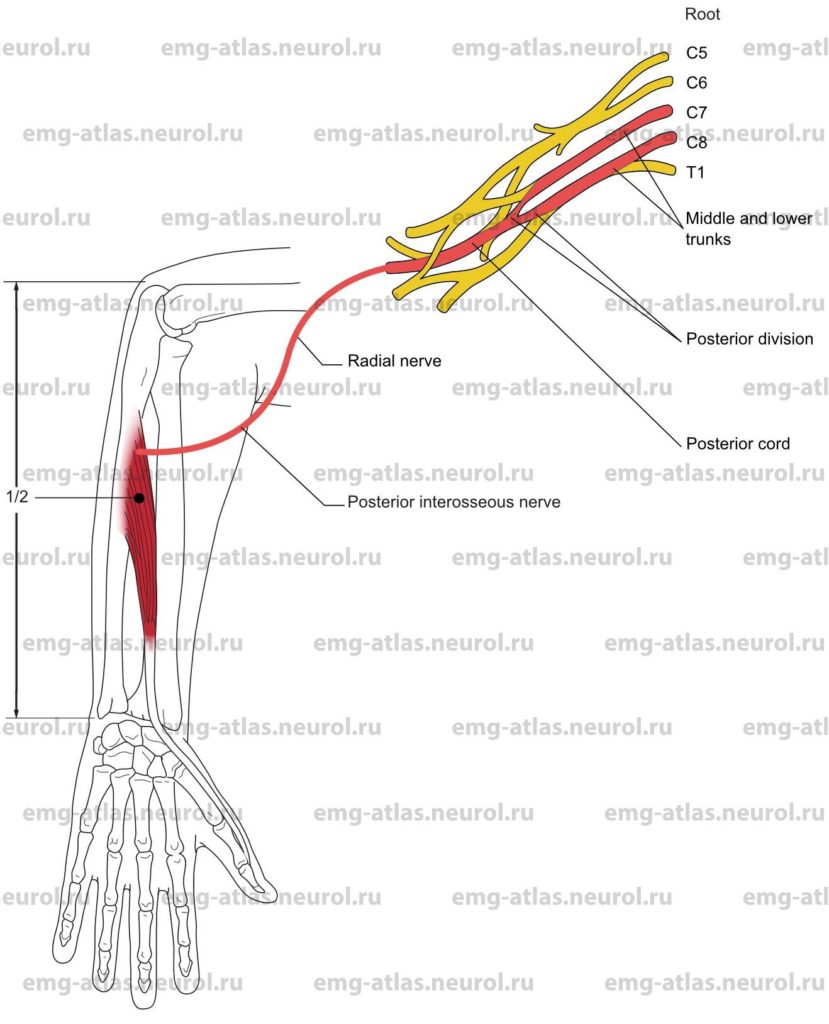
Extensor Pollicis Longus
Innervation is via the posterior interosseous nerve, radial nerve, posterior cord, middle and lower trunks, and roots C7, C8.
Origin
The extensor pollicis longus originates at the posterior surface of the shaft of the ulna, below the origin of the abductor pollicis longus.
Insertion
Insertion is at the base of the terminal phalanx of the thumb. (Note: The tendon forms the ulnar border of the anatomical «snuffbox»)
Activation Maneuver
Extension of the distal phalanx of the thumb activates the muscle. EMG Needle Insertion
Insert the needle at the mid-forearm along the radial border of the ulna.
Pitfalls
If the needle is inserted too proximally or radially, it may be in the abductor pollicis longus, which also receives innervation from the posterior interosseous nerve.
If the needle is inserted too distally, it may be in the extensor indicts, which is also innervated by the posterior interosseous nerve.
Clinical Comments
In a radial nerve lesion at the axilla (crutch neuropathy), needle examination may show neurogenic changes when compression produces axonal loss.
In a radial nerve lesion at the upper arm (Saturday night palsy), needle examination may show neurogenic changes when compression at the spiral groove produces axonal loss.
In a posterior interosseous nerve lesion, needle examination may show neurogenic changes when pathology produces axonal loss.
Anatomical Illustrations
Abductor Pollicis Longus
Innervation
Innervation is via the posterior interosseous nerve, radial nerve, posterior cord, middle and lower trunks, and roots C7, C8.
Origin
The abductor pollicis longus originates at the posterior surface of the shaft of the ulna, above the origin of the extensor pollicis longus; at the posterior surface of the shaft of the radius, above the origin of the extensor pollicis brevis; and at the adjacent interosseous membrane.
Insertion
Insertion is at the base of the metacarpal bone of the thumb. (Note: The tendon forms the radial border of the anatomical «snuffbox»)
Activation Maneuver
Radial abduction and extension of the thumb activate the muscle.
EMG Needle Insertion
Insert the needle at the mid-forearm along the shaft of the radius.
Pitfalls
If the needle is inserted too distally, it may be in the extensor pollicis brevis, which also receives innervation from the posterior interosseous nerve.
If the needle is inserted too proximally, it may be in the extensor carpi radialis, which is innervated by the radial nerve.
If the needle is inserted too medially (ulnarly), it may be in the extensor digitorum communis, which also receives innervation from the posterior interosseous nerve.
Clinical Comments
In a radial nerve lesion at the axilla (crutch neuropathy), needle examination may show neurogenic changes when compression produces axonal loss.
In a radial nerve lesion at the upper arm (Saturday night palsy), needle examination may show neurogenic changes when compression at the spiral groove produces axonal loss.
In a posterior interosseous nerve lesion, needle examination may show neurogenic changes when pathology produces axonal loss.
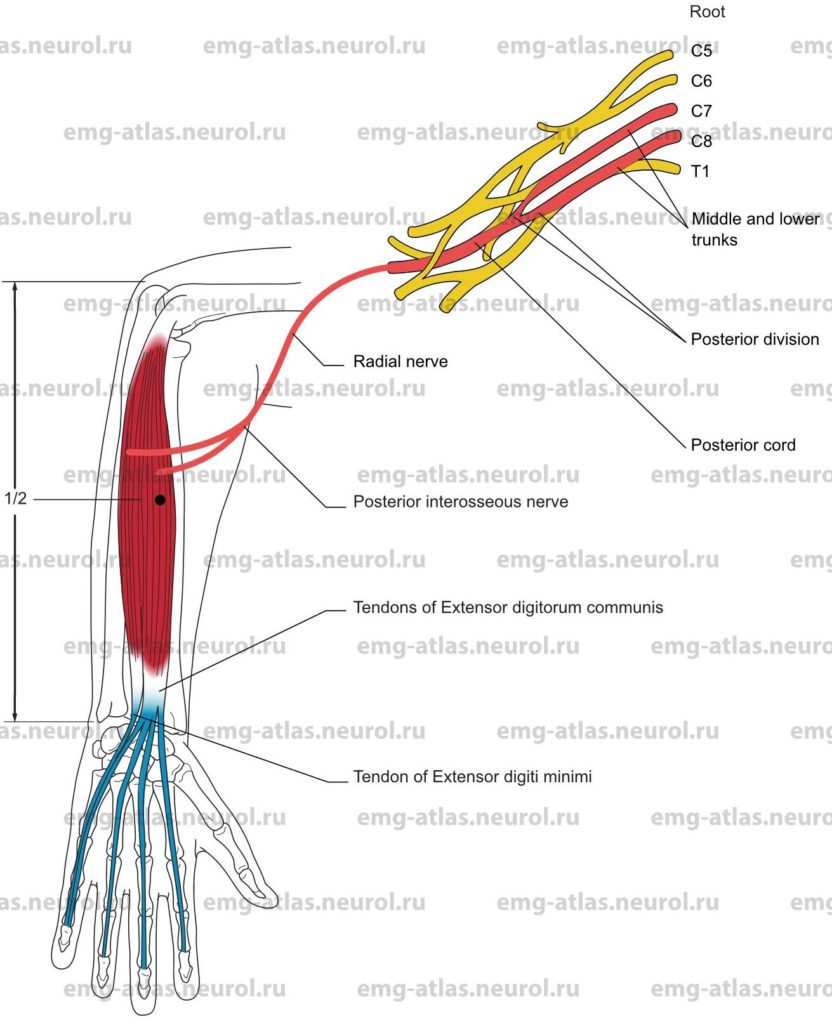
Anatomical Illustrations
Extensor Digitorum Communis and Extensor Digiti Minimi
Innervation
Innervation is via the posterior interosseous nerve, radial nerve, posterior cord, middle and lower trunks, and roots C7, C8.
Origin
The extensor digitorurn communis and extensor digiti minimi originate at the common extensor tendon from the lateral epicondyle of the humerus.
Insertion
Insertion is at the dorsal surface of all phalanges of digits 2 through 5.
Activation Maneuver
Extension of the phalanges in digits 2 through 5 activates the muscles. (Note: These muscles act principally on the proximal phalanges, the middle and distal phalanges being extended by the lumbricals and interossei.)
EMG Needle Insertion
Insert the needle in the mid-forearm midway between the ulna and radius. The extensor digiti minimi is frequently fused with the extensor digitorum communis. The extensor digiti minimi can be found in the mid-forearm on the ulnar border of the extensor digitorum communis.
Pitfalls
If the needle is inserted too laterally (radially), it may be in the extensor carpi radialis, which is innervated by the radial nerve.
If the needle is inserted too medially (ulnarly), it may be in the extensor carpi ulnaris, which also receives innervation from the posterior interosseous nerve.
Clinical Comments
In a radial nerve lesion at the axilla (crutch neuropathy), needle examination may show neurogenic changes when compression produces axonal loss.
In a radial nerve lesion at the upper arm (Saturday night palsy), needle examination may show neurogenic changes when compression at the spiral groove produces axonal loss.
In a posterior interosseous nerve lesion, needle examination may show neurogenic changes when pathology produces axonal loss.
Anatomical Illustrations
Extensor Carpi Ulnaris
Innervation
Innervation is via the posterior interosseous nerve, radial nerve, posterior cord, middle and lower trunks, and roots C7, C8.
Origin
The extensor carpi ulnaris originates at the common extensor tendon from the lateral epicondyle of the humerus.
Insertion
Insertion is at the ulnar side of the base of the fifth metacarpal bone.
Activation Maneuver
Wrist extension with ulnar deviation activates the muscle.
EMG Needle Insertion
Insert the needle in the mid to upper forearm just radial to the lateral margin of the shaft of the ulna.
Pitfalls
If the needle is inserted too laterally (radially), it may be in the extensor digiti minimi or extensor digitorum communis; both are innervated by the posterior interosseous nerve.
Clinical Comments
In a radial nerve lesion at the axilla (crutch neuropathy), needle examination may show neurogenic changes when compression produces axonal loss.
In a radial nerve lesion at the upper arm (Saturday night palsy), needle examination may show neurogenic changes when compression at the spiral groove produces axonal loss.
In a posterior interosseous nerve lesion, needle examination may show neurogenic changes when pathology produces axonal loss.
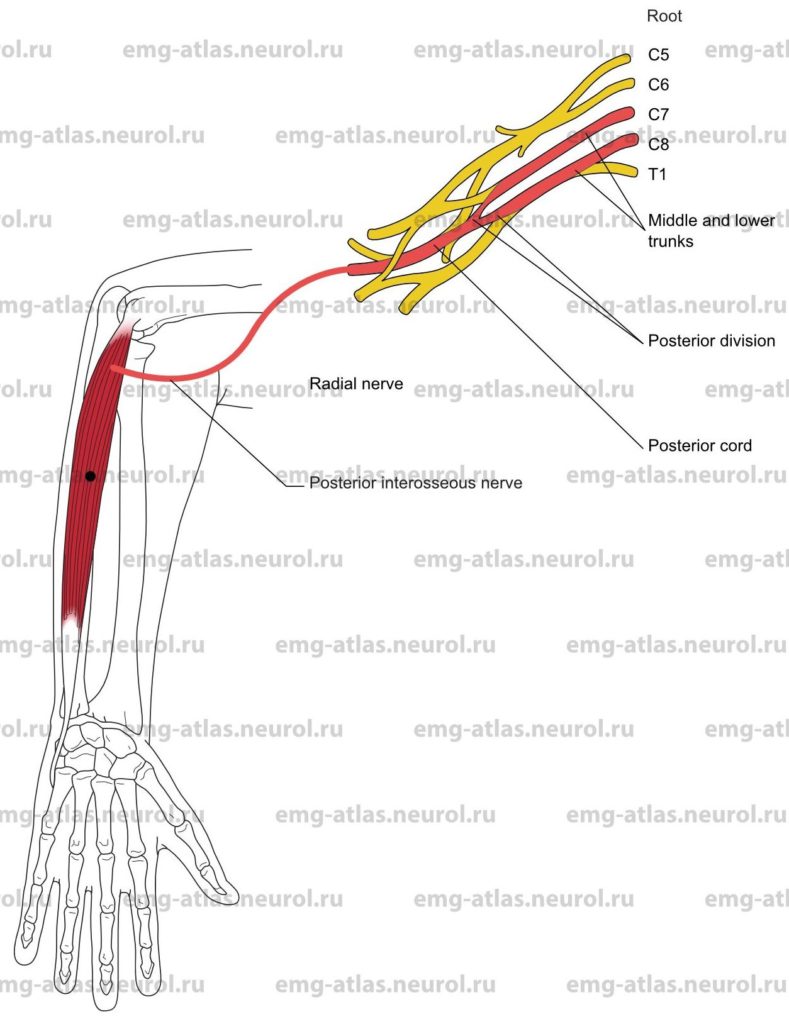
Anatomical Illustrations
Supinator
Innervation
Innervation is via the posterior interosseous nerve, radial nerve, posterior cord, upper trunk, and roots C5, C6.
Origin
The supinator originates at the lateral epicondyle of the humerus, radial collateral ligament of the elbow, and ridge of the ulna.
Insertion
Insertion is at the dorsal and lateral surfaces of upper third of the radius.
Activation Maneuver
Supination of the forearm activates the muscle.
EMG Needle Insertion
With the forearm pronated, insert the needle 3-5 cm distal to the lateral epicondyle, toward the shaft of the radius.
Pitfalls and Clinical Comments
This muscle lies deep. It is rarely of benefit to test it in a routine EMG evaluation.
The posterior interosseous nerve lies between the superficial and deep layers of this muscle in the arcade of Frohse. Entrapment at this site produces the posterior interosseous nerve syndrome, sometimes referred to as the supinator syndrome. The needle examination is usually normal. (Note: The muscle naming a syndrome is usually spared in that syndrome.)
In a radial nerve lesion at the axilla (crutch neuropathy), needle examination may show neurogenic changes when compression produces axonal loss.
In a radial nerve lesion at the upper arm (Saturday night palsy), needle examination may show neurogenic changes when compression at the spiral groove produces axonal loss.
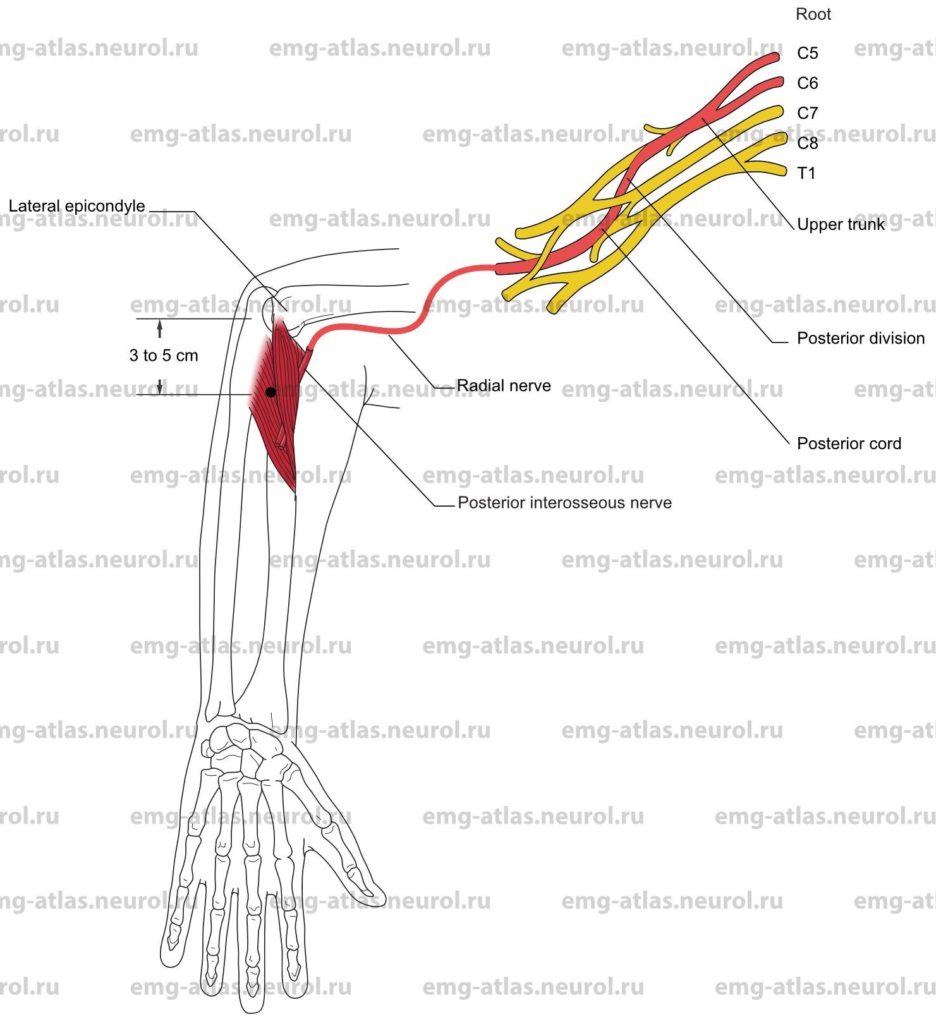
Anatomical Illustrations
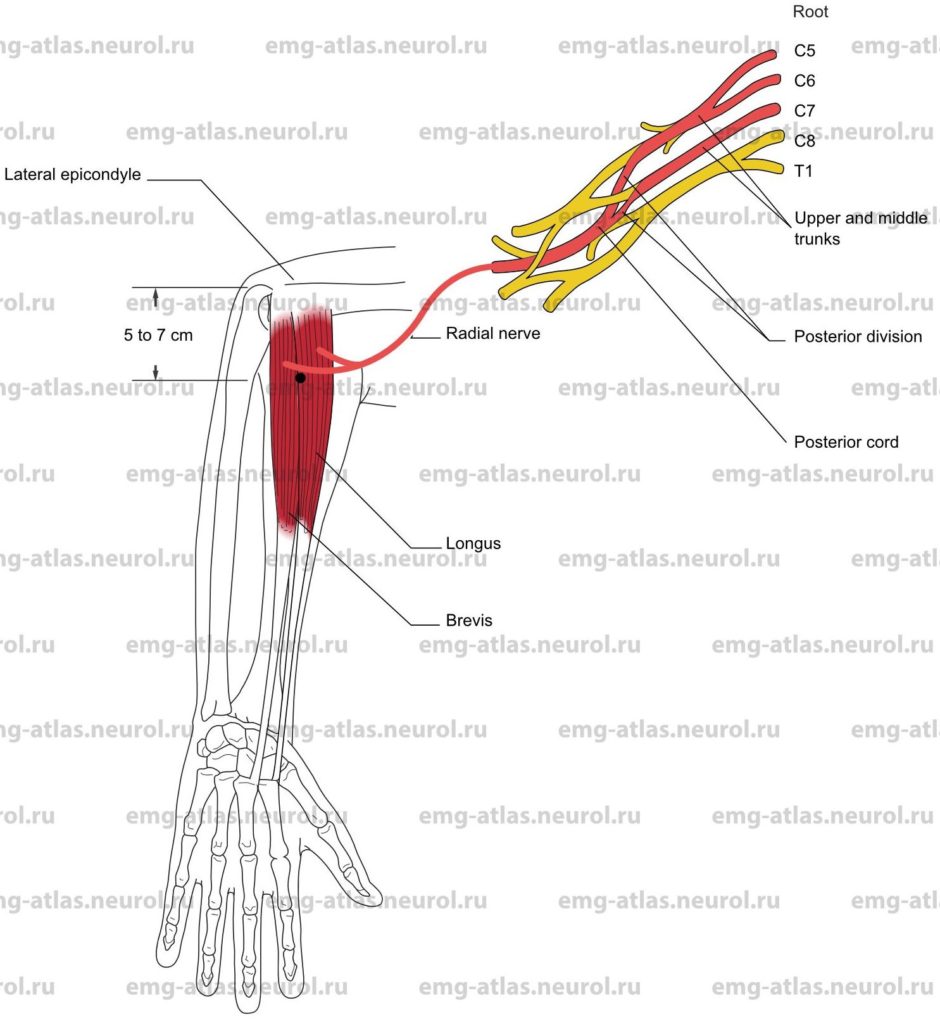
Extensor Carpi Radialis, Longus and Brevis
Innervation
Innervation is via the radial nerve, posterior cord, upper and middle trunks, and roots C5, C6, C7.
Origin
The extensor carpi radialis longus originates at the lower third of the lateral supracondylar ridge of the humerus.
The extensor carpi radials brevis originates at the common extensor tendon from the lateral epicondyle of the humerus.
Insertion
Longus: Insertion is at the radial surface of the base of the second metacarpal bone.
Brevis: Insertion is at the radial surface of the base of the third metacarpal bone.
Activation Maneuver
Extension and radial deviation of the wrist activates the muscles. The activation maneuver should be performed while flexing the digits to avoid coactivatingthe extensor digitorum communis.
EMG Needle Insertion
Insert the needle in the upper forearm 5-7 cm distal to the lateral epicondyle along a line connecting the epicondyle and second metacarpal bone.
Pitfalls
If the needle is inserted too laterally (radially), it may be in the brachioradialis, which is also innervated by the radial nerve.
If the needle is inserted too medially (ulnarly), it may be in the extensor digitorum communis, which receives innervation from the posterior interosseous nerve.
Clinical Comments
In a radial nerve lesion at the axilla (crutch neuropathy), needle examination may show neurogenic changes when compression produces axonal loss.
In a radial nerve lesion at the upper arm (Saturday night palsy), needle examination may show neurogenic changes when compression at the spiral groove produces axonal loss.
In a posterior interosseous nerve lesion, needle examination will be normal.
Anatomical Illustrations
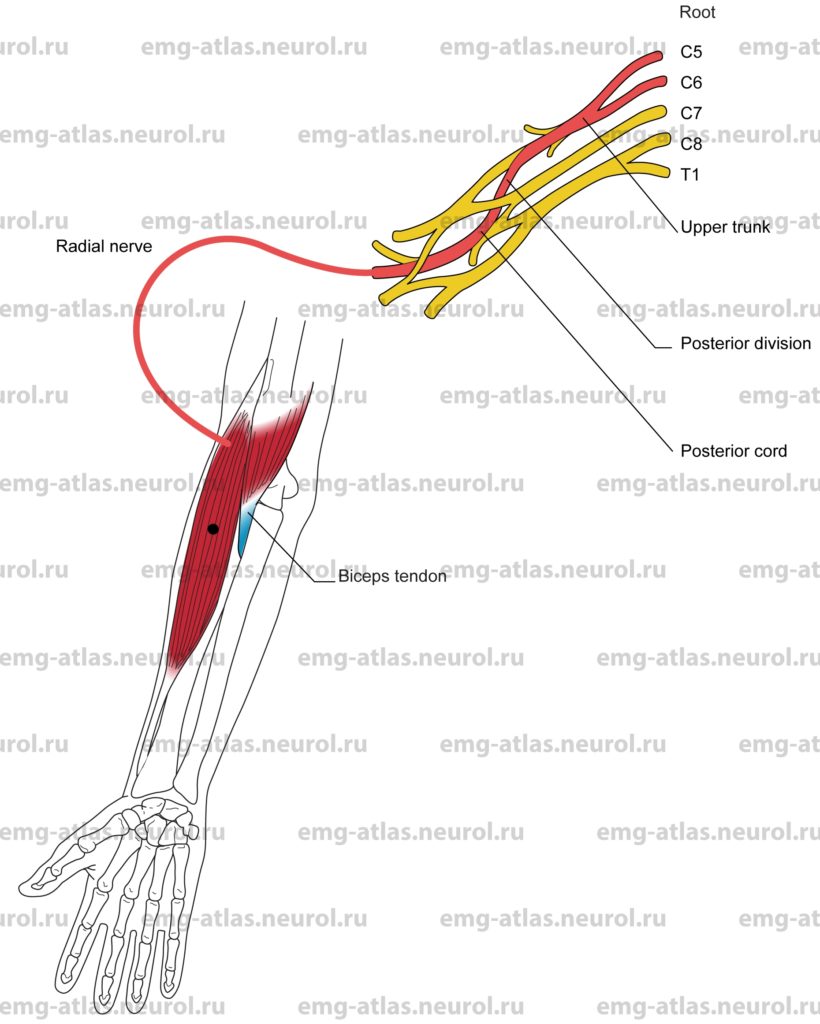
Brachioradialis
Innervation
Innervation is via the radial nerve, posterior cord, upper trunk, and roots C5, C6.
Origin
The brachioradialis originates at the upper two-thirds of the lateral supracondylar ridge of the humerus.
Insertion
Insertion is at the lateral aspect of the base of the styloid process of the radius.
Activation Maneuver
Flexion of the forearm in the neutral position may act both as a supinator or pronator to bring the forearm back to a neutral position) activates the muscle.
EMG Needle Insertion
Insert the needle 2-3 cm lateral to the biceps tendon. The brachiordialis is the first muscle lateral to the biceps tendon.
Pitfalls
If the needle is inserted too laterally (radially), it may be in the extensor carpi radialis, which is also innervated by the radial nerve.
If the needle is inserted too medially (ulnarly) and distally, it may be in the pronator teres, which receives innervation from the median nerve.
Clinical Comments
This muscle is the only major flexor of the elbow joint not innervated by the musculocutaneous nerve.
In a radial nerve lesion at the axilla (crutch neuropathy), needle examination may show neurogenic changes when compression produces axonal loss.
In a radial nerve lesion at the upper arm Saturday night palsy), needle examination may show neurogenic changes when compression at the spiral groove produces axonal loss.
In a posterior interosseous nerve lesion, needle examination will be normal.
Anatomical Illustrations
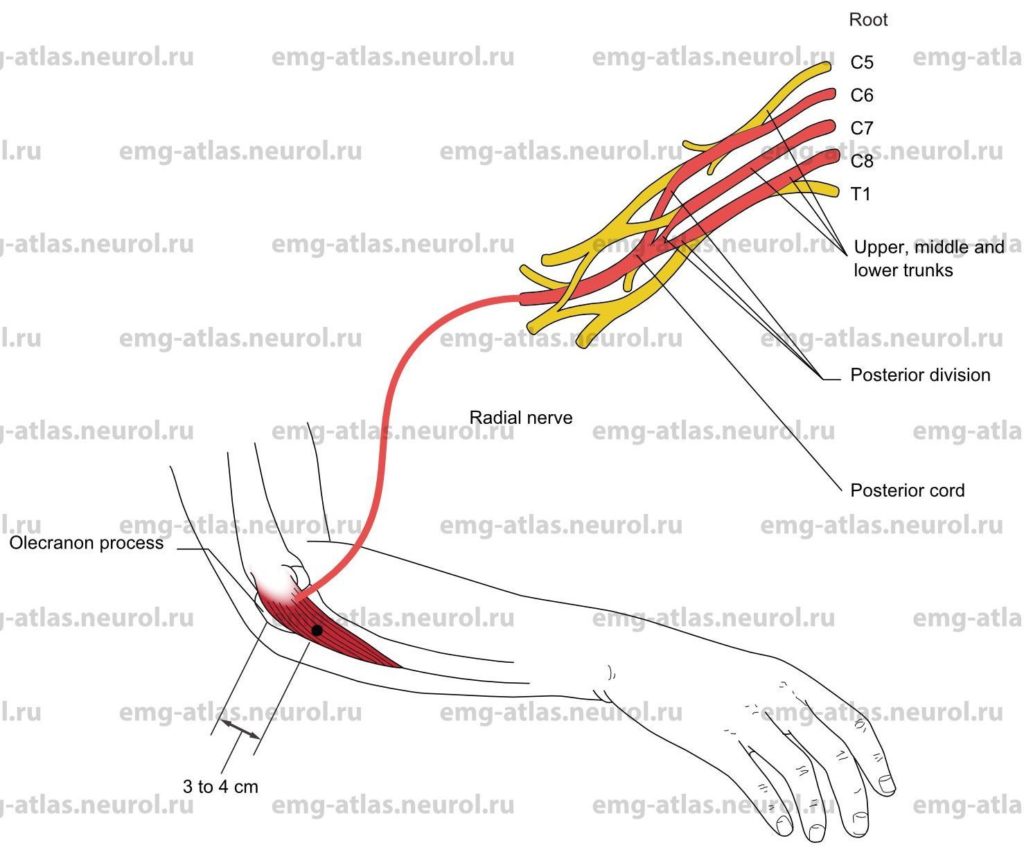
Anconeus
Innervation
Innervation is via the radial nerve; posterior cord; upper, middle, and lower trunks; and roots C6, C7, C8.
Origin
The aconeus originates at the posterior aspect of the lateral epicondyle of the humerus.
Insertion
Insertion is at the lateral aspect of the olecranon process and upper fourth of the posterior surface of the ulna.
Activation Maneuver
Extension of the forearm activates the muscle.
EMG Needle Insertion
Insert the needle 3-4 cm distal to the olecranon along the radial border of the ulna.
Pitfalls
If the needle is inserted along the medial (ulnar) border of the ulna, it may be in the flexor digitorum profundus, which is innervated by the ulnar and median nerves.
If the needle is inserted too radially or distally, it may be in the extensor carpi ulnaris, which receives innervation from the posterior interosseous nerve.
If the needle is inserted too deeply, it may be in the supinator, which receives innervation from the posterior interosseous nerve.
Clinical Comments
The anconeus is a continuation of the medial head of the triceps. It is the only forearm muscle innervated by the radial nerve that is spared in lesions at the upper arm (Saturday night palsy).
In a radial nerve lesion at the axilla (crutch neuropathy), needle examination may show neurogenic changes when compression produces axonal loss.
In a posterior interosseous nerve lesion, needle examination will be normal.
Anatomical Illustrations
Triceps, Lateral Head
Innervation
Innervation is via the radial nerve; posterior cord; upper, middle, and lower trunks; and roots C6, C7, C8.
Origin
The lateral head of the triceps originates in the posterior aspect of the shaft of the humerus.
Insertion
Insertion is at the posterior aspect of the olecranon process of the ulna.
Activation Maneuver
Extension of the forearm at the elbow joint activates the muscle. EMG Needle Insertion
Insert the needle at the midarm level posterior to the lateral aspect of the shaft of the humerus.
Pitfalls
If the needle is inserted too proximally, it may be in the deltoid, which is innervated by the axillary nerve.
If the needle is inserted too anteriorly, it may be in the lateral border of the brachialis or biceps, which are innervated by the musculocutaneous nerve.
Clinical Comments
In a radial nerve lesion at the upper arm (Saturday night palsy), needle examination is almost always normal.
In a radial nerve lesion at the axilla (crutch neuropathy), needle examination may show neurogenic changes when compression produces axonal loss.
In a posterior interosseous nerve lesion, needle examination will be normal.
Anatomical Illustrations
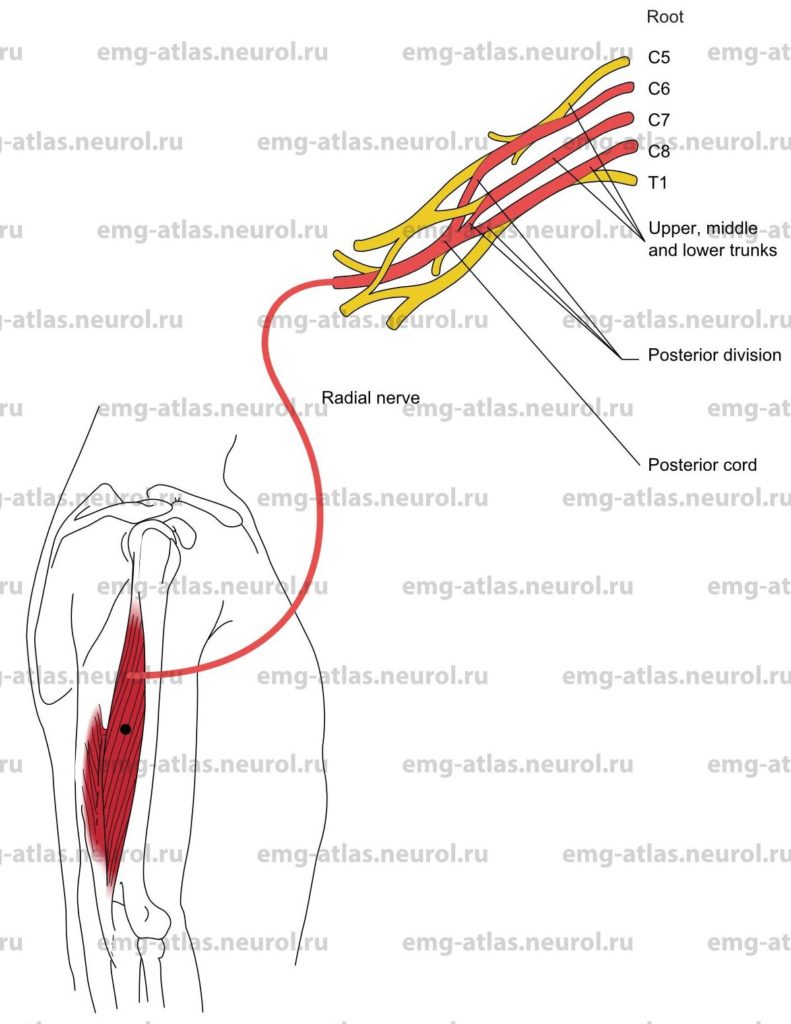
Triceps, Long Head
Innervation
Innervation is via the radial nerve; posterior cord; upper, middle, and lower trunks; and roots C6, C7, C8.
Origin
The long head of the triceps originates at the scapula, immediately below the glenoid cavity.
Insertion
Insertion is at the posterior aspect of the olecranon process of the ulna.
Activation Maneuver
Extension of the forearm at the elbow joint activates the muscle.
EMG Needle Insertion
Insert the needle into the posterior aspect of the arm in the midline, at the junction of the upper and middle thirds of the arm.
Pitfalls
If the needle is inserted too proximally, it may be in the posterior head of the deltoid, which is innervated by the axillary nerve.
Clinical Comments
In a radial nerve lesion at the upper arm (Saturday night palsy), needle examination is almost always normal.
In a radial nerve lesion at the axilla (crutch neuropathy), needle examination may show neurogenic changes when compression produces axonal loss.
In a posterior interosseous nerve lesion, needle examination will be normal.
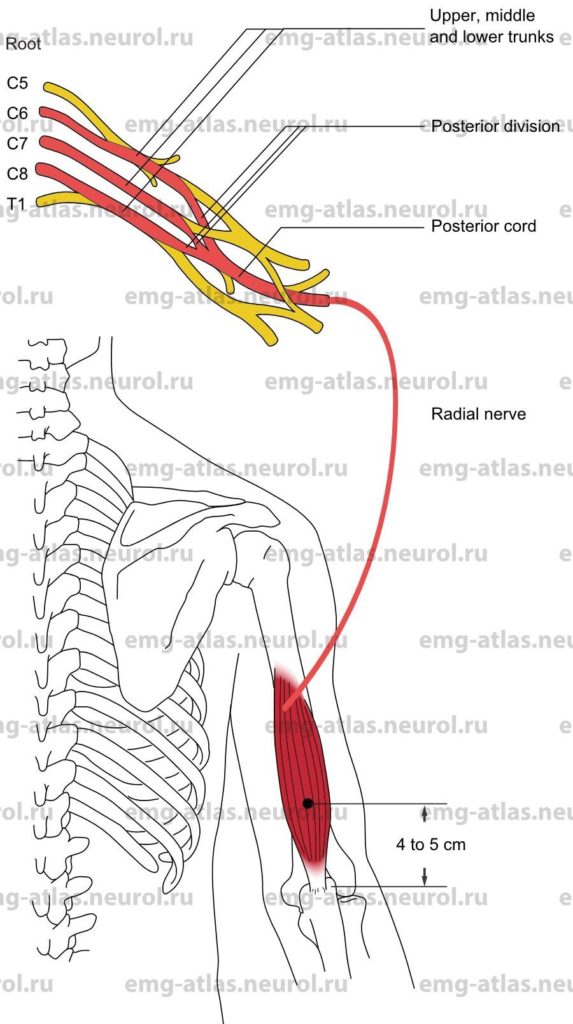
Anatomical Illustrations
Triceps, Medial Head
Innervation
Innervation is via the radial nerve; posterior cord; upper, middle, and lower trunks; and roots C6, C7, C8.
Origin
The medial head originates in the posterior surface of the shaft of the humerus, below the spiral groove.
Insertion
Insertion is at the posterior aspect of the olecranon process of the ulna.
Activation Maneuver
Extension of the forearm at the elbow joint activates the muscle.
EMG Needle Insertion
Insert the needle 4-5 cm proximal to the olecranon process just medial to the shaft of the humerus.
Pitfalls
If the needle is inserted too anteriorly, it may be in the medial border of the brachialis or biceps, which are innervated by the musculocutaneous nerve.
There is a risk of entering the ulnar or median nerves or of puncturing the brachial artery.
Clinical Comments
Testing the medial head of the triceps is rarely of benefit in a routine EMG needle evaluation.
In a radial nerve lesion at the upper arm (Saturday night palsy), needle examination is almost always normal.
In a radial nerve lesion at the axilla (crutch neuropathy), needle examination may show neurogenic changes when compression produces axonal loss.
In a posterior interosseous nerve lesion, needle examination will be normal.