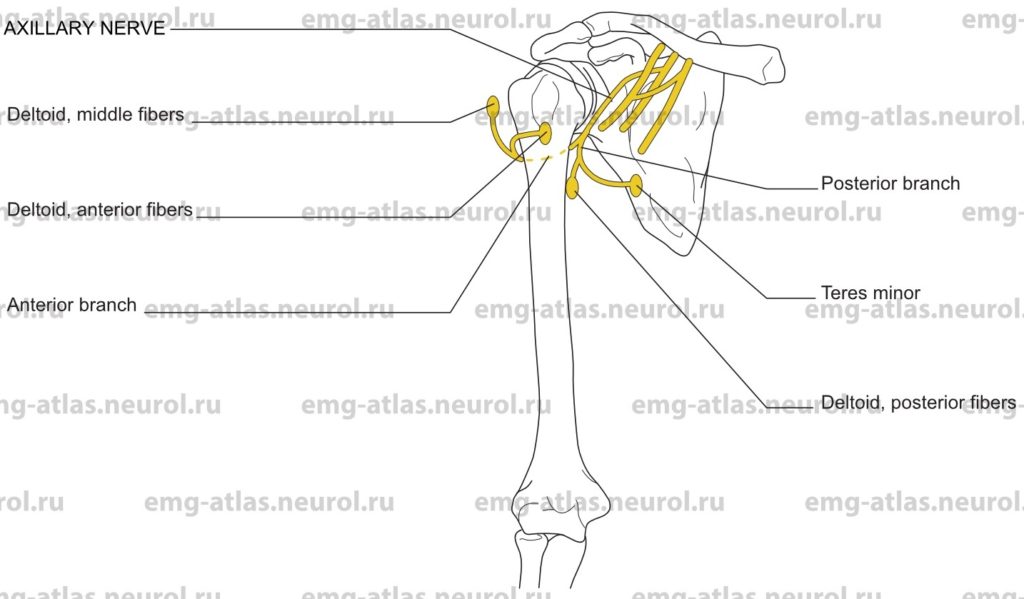
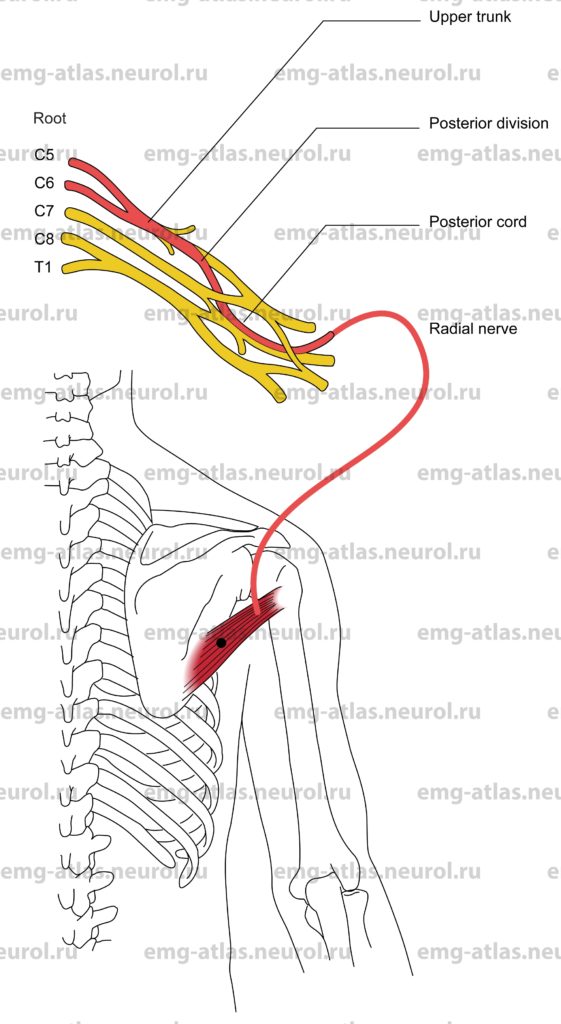
Diagram of the axillary nerve and the muscles that it supplies.
The axillary nerve arises in the axilla as the smaller of the two terminal divisions of the posterior cord. The fibers are derived from the fifth and sixth cervical ventral rami. The nerve descends posteriorto the axillary artery and anterior to the subscapularis muscle. At the lower border of the subscapularis, it curves posteriorly through the quadrangular space with the capsule of the shoulder joint above (humeroscapular articular capsule), the surgical neck of the humerus laterally, the long head of the triceps medially, and the teres major below. In this part of its course it is accompanied by the posterior circumflex artery.
As the nerve emerges from the quadrangular space, it divides into anterior and posteriorterminal divisions. The posterior branch deviates medially and supplies the teres minor and the posterior fibers of the deltoid, which take origin from the spine of the scapula. It then gives off a branch, the upper lateral cutaneous nerve of the arm, to reach and ramify over the skin superficial to the deltoid. The anterior branch turns laterally around the surgical neck of the humerus, accompanied by the posterior circumflex artery. It then supplies the middle and anterior fibers of the deltoid, which take origin from the acromion and clavicle, respectively.
Axillary Nerve Lesion
Etiology
An axillary nerve lesion can occur secondary to inferior dislocation of the humerus at the shoulder joint (the nerve is stretched across the head of the humerus).
An axillary nerve lesion can occur secondary to fractures of the surgical neck of the humerus.
Deep penetrating wounds and upward pressure in the axilla from misused crutches, which also compress the radial nerve (Sunderland, 1968), can cause an axillary nerve lesion.
Neuralgic amyotrophy (brachial plexopathy) can be causative.
General Comments
The most common lesions are those associated with injuries about the shoulder joint.
Clinical Features
Wasting and weakness of the deltoid are present. In the early stages following injury, the arm may hang uselessly by the side. Later, the supplementary actions of other shoulder girdle muscles, including supraspinatus, may result in abduction of the arm even in the absence of deltoid function (Sunderland, 1968).
There is a patch of sensory loss over the outer aspect of the upper arm.
Weakness of the teres minor is not easily demonstrated because other unaffected muscles, such as the infraspinatus, perform the same action.
Most lesions resolve spontaneously.
Electrodiagnostic Strategy
Demonstrate neurogenic EMG changes limited to the deltoid and teres minor.
EMG of nonaxillary innervated C5, C6 muscles may be necessary to exclude cervical radiculopathy.
Motor conduction studies may show reduced amplitude on the affected side.
Anatomical Illustrations
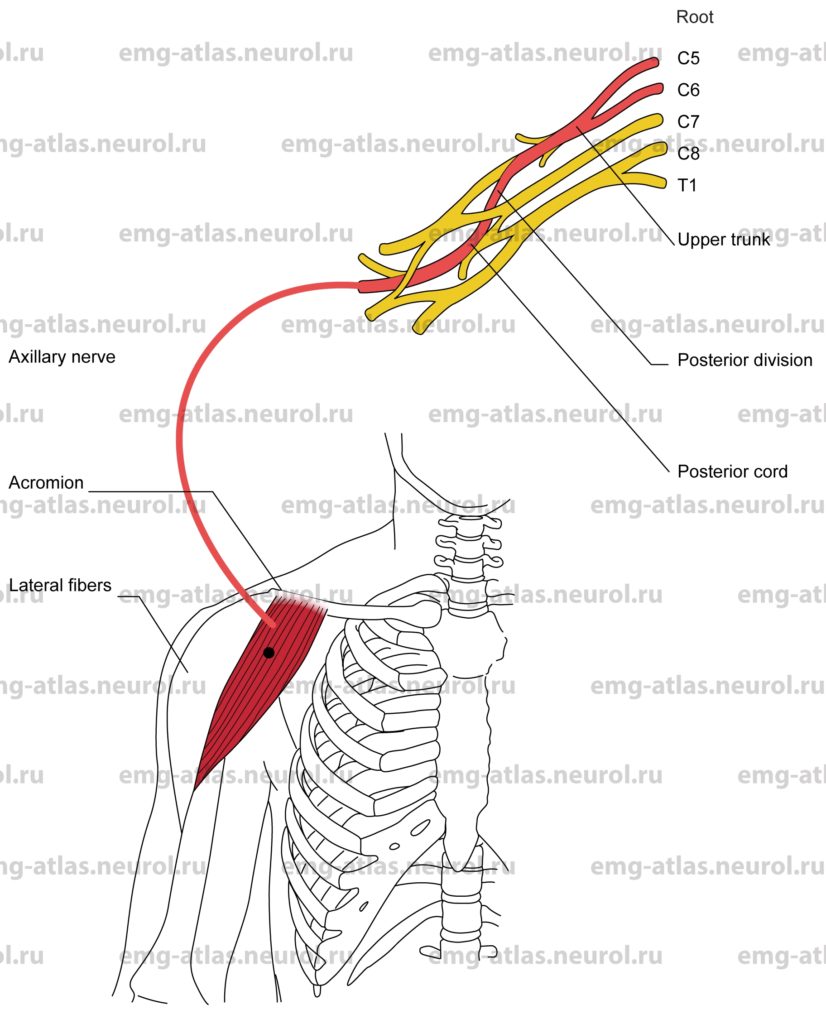
Deltoid, Anterior Fibers
Innervation
Innervation is via the axillary nerve, posterior cord, upper trunk and roots C5, C6.
Origin
The anterior fibers of the deltoid originate at the anterior border and superior surface of the lateral third of the clavicle.
Insertion
Insertion is at the deltoid tuberosity on the lateral aspect of the humerus midshaft.
Activation Maneuver
Forward flexion and medial rotation of the arm activate the anterior fibers of the deltoid (the anterior fibers are assisted by the pectoralis major and coracobrachialis).
EMG Needle Insertion
Insert the needle 3–4 cm directly beneath the anterior margin of the acromion.
Pitfalls
If the needle is inserted too deeply, it may be in the coracobrachialis or tendon of the short head of the biceps. These muscles are supplied by the musculocutaneous nerve.
If the needle is inserted too medially, it may be in the clavicular portion of the pectoralis major, supplied by the medial and lateral pectoral nerves.
Clinical Comments
Needle examination may show neurogenic changes when injury to the axillary nerve produces axonal loss (i.e., blunt trauma, fracture or dislocation of the head of the humerus, brachial plexopathy).
In C5, C6 radiculopathy, needle examination may show neurogenic changes when root pathology has resulted in axonal loss (i.e., in moderate to severe radiculopathy).
In Erb’s palsy (C5, C6 root avulsion), needle examination will show neurogenic changes.
Anatomical Illustrations
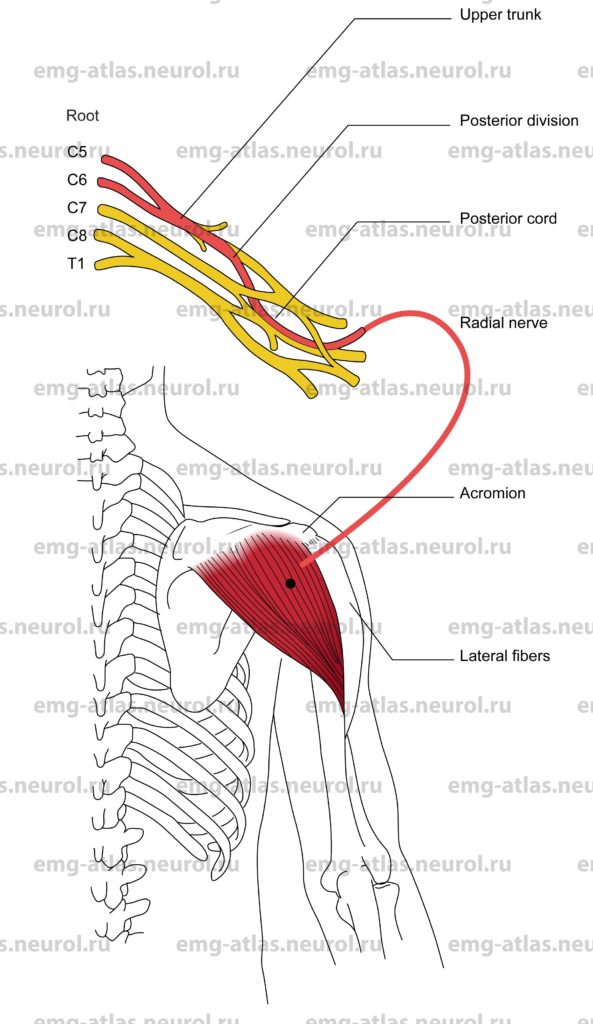
Deltoid, Middle Fibers
Innervation
Innervation is via the axillary nerve, posterior cord, upper trunk, and roots C5, C6.
Origin
The middle fibers of the deltoid originate in the lateral margin and superior surface of the acromion.
Insertion
Insertion is at the deltoid tuberosity on the lateral aspect of the humerus midshaft.
Activation Maneuver
Abduction of the arm activates the middle fibers of the deltoid (the middle fibers are assisted by the supraspintus).
EMG Needle Insertion
Insert the needle 4-5 cm directly beneath the lateral border of the acromion.
Pitfalls
There are no pitfalls.
Clinical Comments
Needle examination may show neurogenic changes when injury to the axillary nerve produces axonal loss (i.e., blunt trauma, fracture or dislocation of the head of the humerus, brachial plexopathy).
A history of multiple intramuscular injections into this muscle may confound needle findings.
In C5, C6 radiculopathy, needle examination may show neurogenic changes when root pathology has resulted in axonal loss (i.e., in moderate to severe radiculopathy).
In Erb’s palsy (C5, C6 root avulsion), needle examination will show neurogenic changes.
Anatomical Illustrations
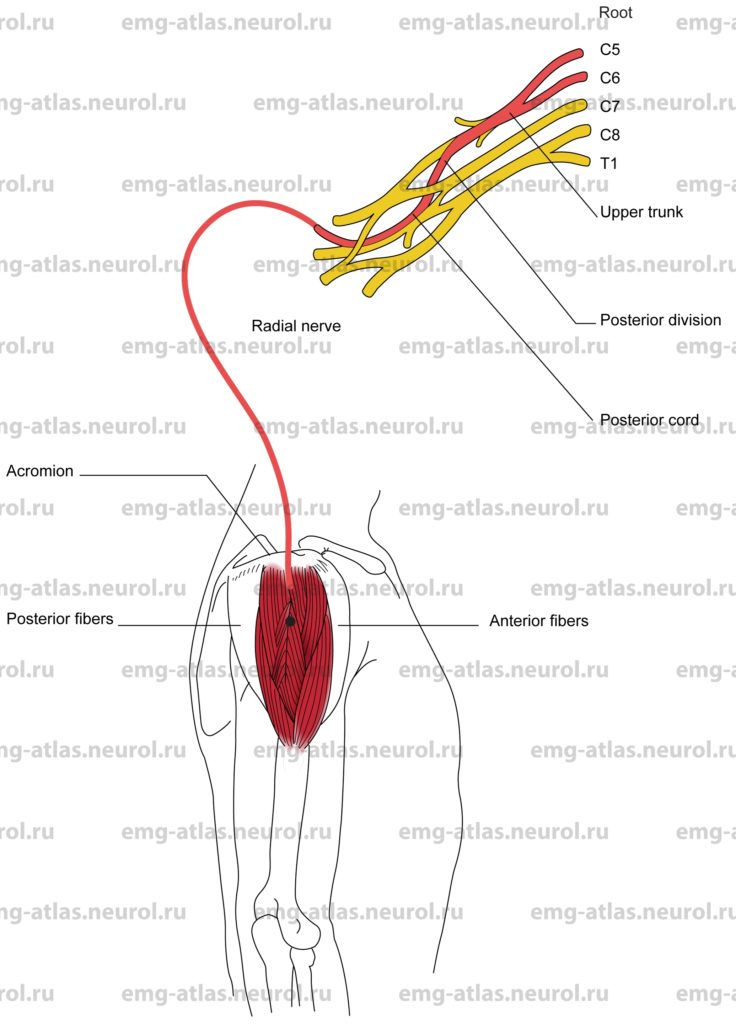
Deltoid, Posterior Fibers
Innervation
Innervation is via the axillary nerve, posterior cord, upper trunk, and roots C5, C6.
Origin
The posterior fibers of the deltoid originate at the lower edge of the crest of the spine of the scapula.
Insertion
Insertion is at the deltoid tuberosity of the humerus.
Activation Maneuver
Backward extension and lateral rotation of the arm activate the posterior fibers of the deltoid (the posterior fibers are assisted in backward extension by the latissimus dorsi and teres major).
EMG Needle Insertion
Insert the needle 3-4 cm directly beneath the posterior margin of the acromion.
Pitfalls
If the needle is inserted too deeply, it may be in the teres minor or the long head of the triceps, which are innervated by the axillary and radial nerves, respectively.
If the needle is inserted too medially, it may be in the infraspinatus, which is innervated by the suprascapular nerve.
Clinical Comments
Needle examination may show neurogenic changes when injury to the axillary nerve produces axonal loss, (i.e., blunt trauma, fracture or dislocation of the head of the humerus, brachial plexopathy).
In C5, C6 radiculopathy, needle examination may show neurogenic changes when root pathology has resulted in axonal loss (i.e., in moderate to severe radiculopathy).
In Erb’s palsy (C5, C6 root avulsion), needle examination will show neurogenic changes.
Anatomical Illustrations
Teres Minor
Innervation
Innervation is via the axillary nerve, posterior cord, upper trunk, and roots C5, C6.
Origin
The teres minor originates in the upper two-thirds of the dorsolateral surface of the scapula.
Insertion
Insertion is at the lowest facet on the greater tubercle of the humerus.
Activation Maneuver
Lateral rotation of the arm (assisted by infraspinatus and posterior fibers of deltoid) activates the muscle.
EMG Needle Insertion
Insert the needle immediately lateral to the middle third of the lateral border of the scapula.
Pitfalls
If the needle is inserted too superficially, it may be in the posterior deltoid, which is also supplied by the axillary nerve.
If the needle is inserted too medially or rostrally, it may be in the infraspinatus, which is innervated by the suprascapular nerve. (Note: The teres minor is sometimes fused with the infraspinatus.)
Clinical Comments
Needle examination may show neurogenic changes when injury to the axillary nerve produces axonal loss (i.e., blunt trauma, fracture or dislocation of the head of the humerus, brachial plexopathy).
In C5, C6 radiculopathy, needle examination may show neurogenic changes when root pathology has resulted in axonal loss (i.e., in moderate to severe radiculopathy).
In Erb’s palsy (C5, C6 root avulsion), needle examination will show neurogenic changes.