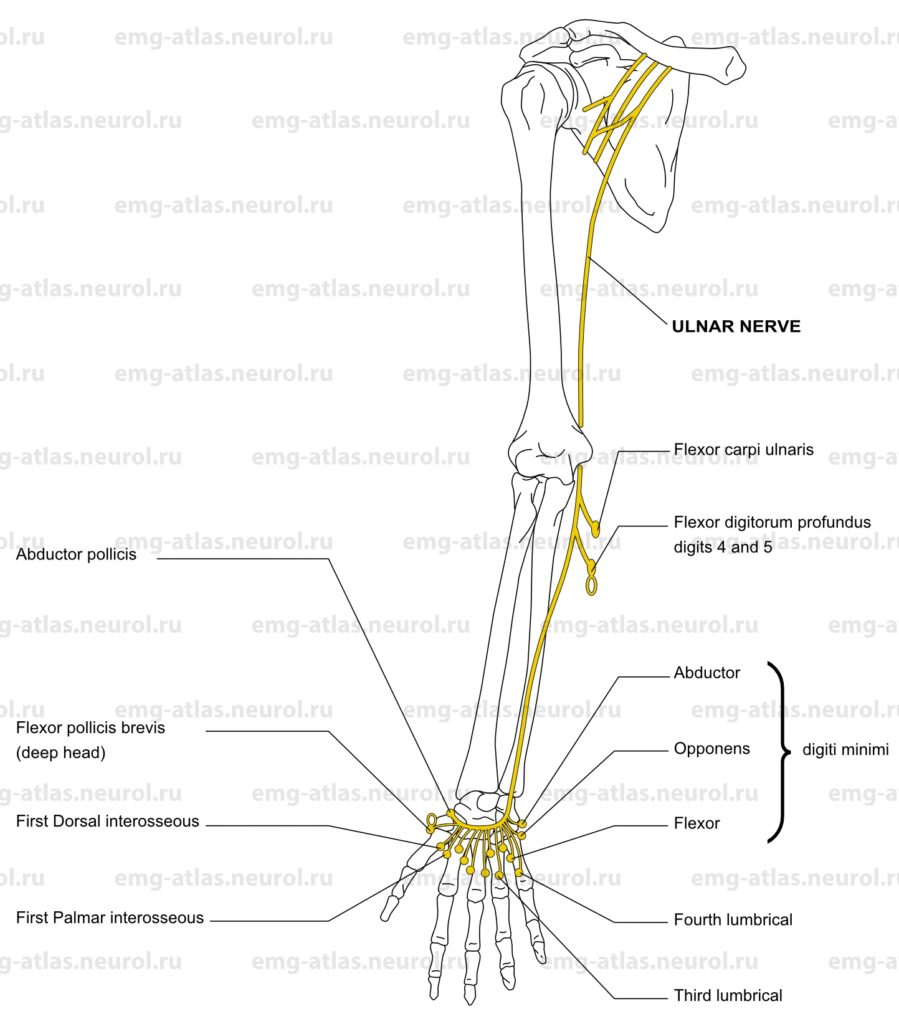
Diagram of the ulnar nerve and the muscles that it supplies. NOTE: The white oval signifies that a muscle receives a part of its innervation from another peripheral nerve.
The ulnar nerve is the main continuation of the medial cord of the brachial plexus. Its fibers are usually derived from the eighth cervical and first thoracic roots, although occasionally the seventh cervical root makes a contribution via the lateral cord (Gray’s Anatomy, 1995). In the axilla, the nerve runs between the axillary artery and vein. In the arm, it stays between the brachial artery and vein, sharing the neurovascular bundle with the median nerve. At the midarm, it leaves the neurovascular bundle and passes posteriorly through the medial intermuscular septum to descend on the medial aspect of the medial head of the triceps. The nerve is superficial throughout this course and innervates no muscles in the arm.
At the elbow, the nerve lies in a groove formed by the medial epicondyle of the humerus and the olecranon process of the ulna (the retrocondylar groove). It enters the forearm through an aponeurotic arcade (the cubital tunnel) joining the two heads of the flexor carpi ulnaris, which it innervates. The arcade typically lies about 1.5 cm distal to the medial epicondyle (Campbell, 1989). The nerve travels through the belly of the flexor carpi ulnaris and then exits by piercing the aponeurosis on the undersurface of the muscle. It then lies in the plane between the flexor carpi ulnaris and the flexor digitorum profundus (to digits 4 and 5), which it innervates.
The nerve is joined by the ulnar artery in the upper forearm to form a neurovascular bundle. About the middle of the forearm, the ulnar nerve gives rise to the palmar cutaneous branch, which descends to provide sensory innervation to the medial aspect of the proximal palm. About 7 cm proximal to the wrist it also gives off a dorsal cutaneous branch, which provides innervation to the medial aspect of the dorsum of the hand and the dorsoproximal aspect of the fifth and medial fourth digits. The ulnar nerve provides no sensory innervation above the wrist. Hence, sensory loss in the forearm or arm is not a feature of an ulnar nerve lesion.
At the wrist, the ulnar nerve and artery lie in a canal formed by the pisiform medially and the hook of the hamate laterally (Guyon’s canal). In this region the nerve divides into superficial and deep branches. Although the superficial branch is generally considered a sensory branch, it supplies the palmaris brevis, a thin muscle beneath the skin of the proximal medial palm, which cannot be studied electromyographically. It then provides sensory innervation to the distal palm and terminates in two digital branches that are distributed to the ulnar side of the fifth digit and the adjoining sides of the fourth and fifth digits. The deep muscular branch gives off a hypothenar branch to innervate the abductor, opponens, and flexor digit minimi. It then follows the course of the deep palmar arch across the hand. As it crosses, it supplies dorsal and palmar interossei and the third and fourth lumbricals. At its termination between the thumb and index fingers, it supplies the flexor pollicis brevis (deep head) and adductor pollicis.
Although the ulnar nerve, or its branches, may be involved by penetrating injuries at any level, there are certain sites where the nerve is prone to injury (Sunderland, 1968). Compression neuropathies of the ulnar nerve at the elbow are common and widely recognized. In the retrocondylar groove, the nerve lies on bone covered only by a thin layer of skin and is subject to chronic compression from multiple etiologies. At 1–2 cm distally, the nerve may be entrapped at the cubital tunnel. Compression at either site may result in the clinical presentation known as ulnar neuropathy at the elbow. Rarely, the nerve may be entrapped in the proximal forearm as it pierces the deep aponeurosis investing the undersurface of the flexor carpi ulnaris (Amadio and Beckenbaugh, 1986; Campbell et al., 1988) or in the distal forearm by a fibrovascular band or hypertrophied flexor carpi ulnaris tendon (Campbell, 1989). Entrapment at the wrist (Guyon’s canal) may present with different patterns of sensorimotor deficits, depending on the degree of involvement of the superficial (sensory) or deep (motor) branches.
Ulnar Neuropathy at the Elbow (Retrocondylar Groove)
Etiology
Ulnar neuropathy at the elbow can be caused by compression at the retrocondylar groove due to repeated trauma (habitual leaning on the elbows), traumatic joint deformity, distal humerus fractures, elbow dislocations, recurrent subluxation of the nerve, callus formation, rheumatic and degenerative joint disease, congenital anomalies of the medial epicondyle, epicondylo-olecranon ligament, valgus deformity, and immobilization during surgery.
General Comments
Originally, the term tardy ulnar palsy referred to antecedent traumatic joint deformity or recurrent subluxation. Many clinicians now use the term for any entrapment of the ulnar nerve at the elbow.
The appearance of ulnar mononeuropathy may herald the onset of a more generalized neuropathy.
Ulnar neuropathy at the retrocondylar groove should be distinguished electrodiagnostically from cubital tunnel syndrome. The distinction can be important in surgical management; the former generally requires surgical transposition of the nerve, whereas the latter may warrant simple decompression of the nerve in the tunnel, without transposition (Miller, 1991).
Clinical Features
Paresthesia, pain, or numbness occurs in the sensory distribution of the ulnar nerve, including the dorsum of the hand.
There is pain or tenderness at the elbow.
Weakness and wasting of the first dorsal interosseous and other ulnarinnervated hand muscles may occur in severe cases. Clinical evidence of weakness may preferentially involve the first dorsal interosseous (Stewart, 1987).
Weakness of the flexor carpi ulnaris and flexor digitorum profundus (to digits 4 and 5) may be variable.
Radiographic studies may visualize rheumatic, arthritic, or post-traumatic changes around the elbow.
Electrodiagnostic Strategy
Use special nerve conduction studies («inching technique») to precisely localize the conduction abnormality (focal slowing, conduction block) to the retrocondylar region.
Use routine nerve conduction studies to demonstrate an absent or reduced ulnar dorsal cutaneous response.
Demonstrate neurogenic EMG abnormalities in the first dorsal interosseous and other ulnar-innervated hand muscles.
EMG abnormalities in the flexor carpi ulnaris and flexor digitorum profundus (superficial head) localize the lesion to the elbow. In many patients, however, these muscles may be normal, however particularly in mild ulnar neuropathy (Kincaid, 1988; Campbell et al., 1989).
Ulnar Neuropathy at the Elbow (Cubital Tunnel Syndrome)
Etiology
Entrapment of the ulnar nerve occurs in the tunnel formed by the tendinous arch connecting the humeral and ulnar heads of the flexor carpi ulnaris 1-2 cm distal to the medial epicondyle.
General Comments
The cubital tunnel narrows when the elbow is flexed, this is important in the development of this compression neuropathy.
There is no joint deformity or prior trauma to the elbow.
Bilateral ulnar neuropathy occurs frequently.
Ulnar neuropathy at the retrocondylar groove should be distinguished electrodiagnostically from cubital tunnel syndrome. The former generally requires surgical transposition of the nerve, whereas the latter may warrant simple decompression in the tunnel, without transposition (Miller, 1991).
Clinical Features
Paresthesia, pain, or numbness occurs in the sensory distribution of the ulnar nerve, including the dorsum of the hand.
There is pain or tenderness at or slightly distal to the elbow.
In severe cases, weakness and wasting of the first dorsal interosseous and other ulnar-innervated hand muscles may occur. Clinical evidence of weakness may preferentially involve the first dorsal interosseous (Stewart, 1987).
Weakness of the flexor carpi ulnaris and flexor digitorum profundus (to digits 4 and 5) may be variable.
Radiographic studies are normal.
Electrodiagnostic Strategy
Use special nerve conduction studies («inching technique») to precisely localize the conduction abnormality (focal slowing, conduction block) to the cubital tunnel.
Use routine nerve conduction studies to demonstrate an absent or reduced ulnar dorsal cutaneous response.
Demonstrate neurogenic EMG abnormalities in the first dorsal interosseous and other ulnar-innervated hand muscles.
EMG abnormalities in the flexor carpi ulnaris and flexor digitorum (profundus superficial head) localize the lesion to the elbow. These muscles may be normal, however, particularly in mild ulnar neuropathy (Kincaid, 1988; Campbell et al., 1989).
Ulnar Neuropathy at the Wrist (Guyon’s Canal)
Etiology
Entrapment of the ulnar nerve occurs in the tunnel formed by the pisiform bone medially and the hook of the hamate laterally. The firm floor consists of the thick transverse carpal ligament and subjacent bone. The distal roof is rigidly bound by the piso-hamate ligament.
Entrapment may be associated with a lipoma, ganglion cyst, aneurysm, other mass lesion, or chronic compression to the hypothenar region (bicycle bars, crutches, occupation).
General Comments
Within the canal, the nerve divides into superficial (sensory) and deep (muscular) branches.
Clinical Features
Nerve or branch lesions at four different locations within Guyon’s canal produce distinctive patterns of symptoms and signs (Olney and Hanson, 1988).
Pattern 1: A deep branch lesion distal to the hypothenar motor branch produces weakness in the interossei and lumbricals but not the hypothenar muscles; there are no sensory deficits.
Pattern 2: A lesion at or proximal to hypothenar motor branch produces weakness in the interossei, lumbricals, and hypothenar muscles; there are no sensory deficits.
Pattern 3: A lesion at or proximal to the bifurcation into deep and superficial branches produces weakness in the interossei, lumbricals, and hypothenar muscles and sensory deficits in the distal palm, fifth digit, and ulnar side of the fourth digit.
Pattern 4: A lesion limited to the superficial branch produces only sensory deficits in the distal palm, fifth digit, and ulnar side of the fourth digit.
Lesions that compress the deep motor branch (patterns 1 and 2) are the most common and may be confused with focaf onset of amyotrophic lateral sclerosis, particularly in the all-ulnar hand.
Lesions that compress the superficial branch (patterns 3 and 4) do not produce loss of sensation over the ulnar dorsal surface of the hand (ulnar dorsal cutaneous distribution).
Electrodiagnostic Strategy
Use nerve conduction studies to localize the conduction abnormality (prolonged distal latencies in motor or sensory responses, reduced amplitudes) to the wrist. Motor conduction studies should record over the first dorsal interosseous as well as hypothenar muscles. This allows detection of distal deep branch lesions.
Elicit normal sensory nerve conduction studies of the ulnar dorsal cutaneous branch.
Demonstrate neurogenic EMG abnormalities in the first dorsal interosseous and other ulnar-innervated hand muscles.
Perform EMG in additional muscles to exclude anterior horn cell disease and C8, T1 radiculopathy.
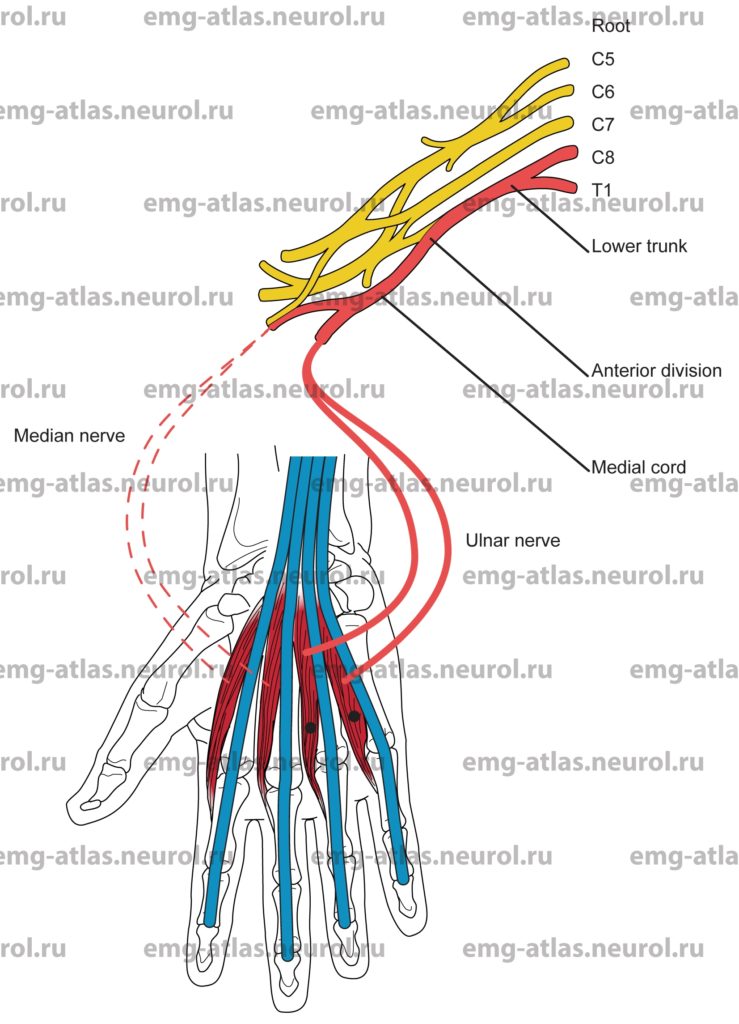
Anatomical Illustrations
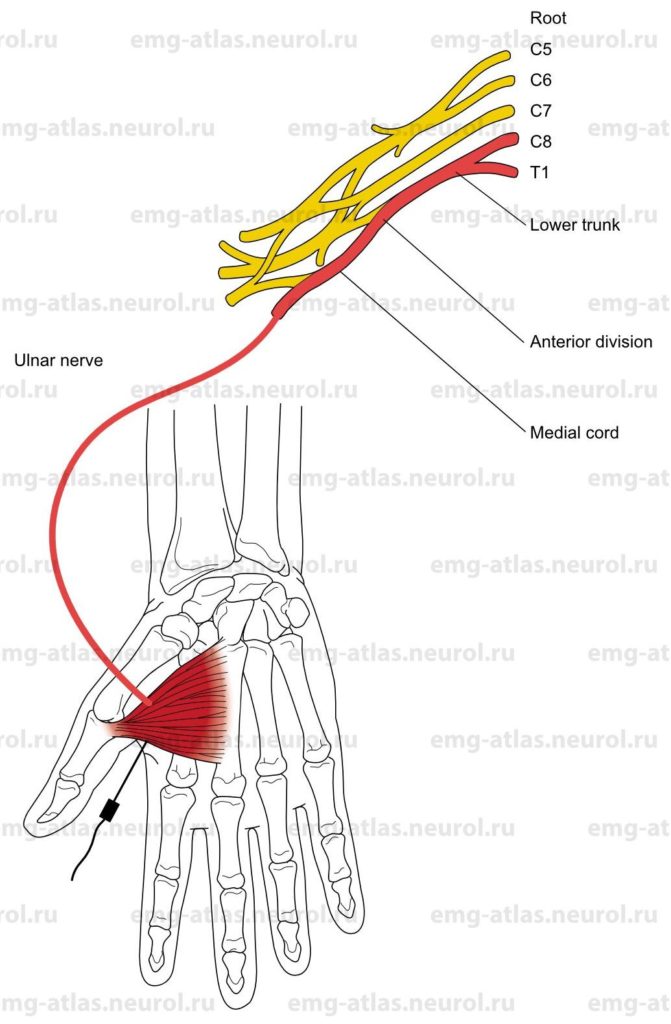
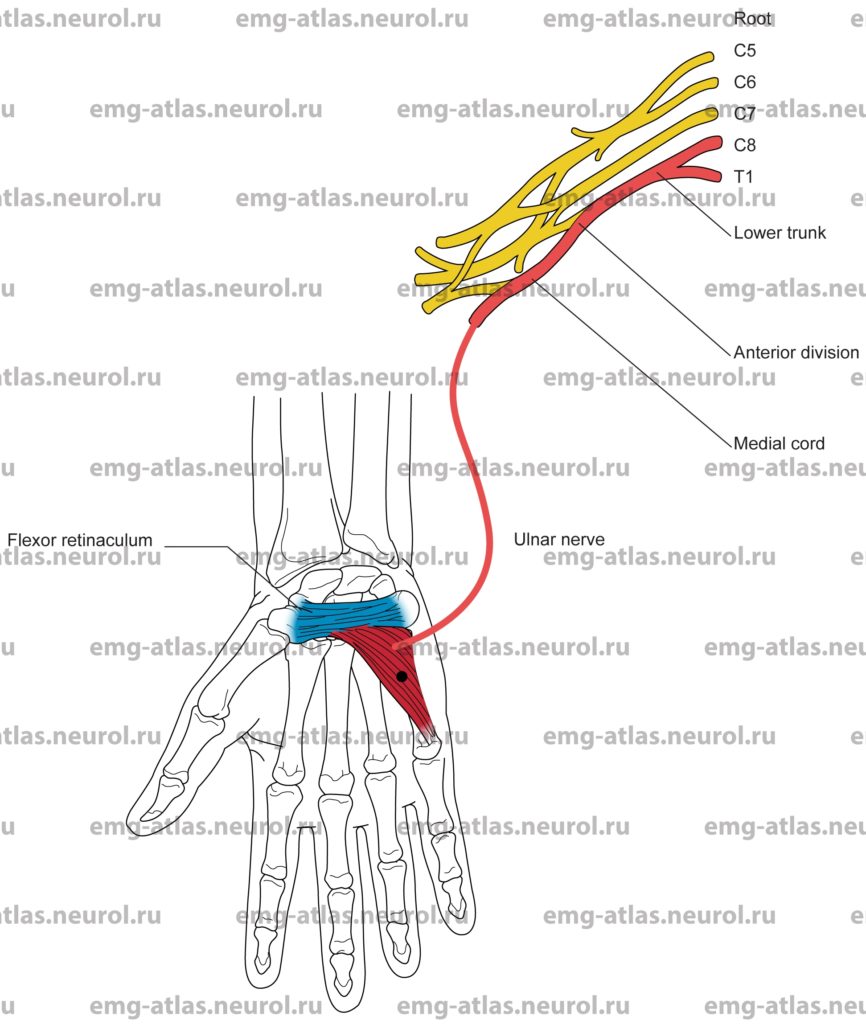
Adductor Pollicis
Innervation
Innervation is via the ulnar nerve, medial cord, lower trunk, and roots C8, T1.
Origin
Oblique fibers arise from the capitate bone and bases of the second and third metacarpal bones; transverse fibers arise from the distal two-thirds of the metacarpal bone of the middle finger.
Insertion
Insertion is at the medial side of the base of the proximal phalanx of the thumb.
Activation Maneuver
Adduction of the thumb activates the adductor pollicis.
EMG Needle Insertion
Insert the needle into the first web space just anterior (volar) to the edge of the first dorsal interosseous and proximal to the first metacarpophalangeal joint.
Pitfalls
If the needle is inserted too posteriorly (dorsaly), it will be in the first dorsal interosseous, which is also supplied by the ulnar nerve.
If the needle is inserted too anteriorly (volarly) and proximally, it may be in thenar muscles innervated by the median nerve.
Clinical Comments
This is the most distal muscle innervated by the ulnar nerve.
If ulnar-innervated muscles are atrophied, the needle is more likely to enter median-innervated thenar muscles.
In ulnar neuropathy at the wrist (Guyon’s canal) or elbow (cubital tunnel, retrocondylar groove), the needle examination may show neurogenic changes when compression produces axonal loss (i.e., in moderate to severe entrapment).
In C8, T1, radiculopathy, the needle examination may show neurogenic changes when root pathology produces axonal loss (i.e., in moderate to severe radiculopathy).
In Klumpke’s palsy (C8, T1, root avulsion), needle examination will show neurogenic changes.
Anatomical Illustrations
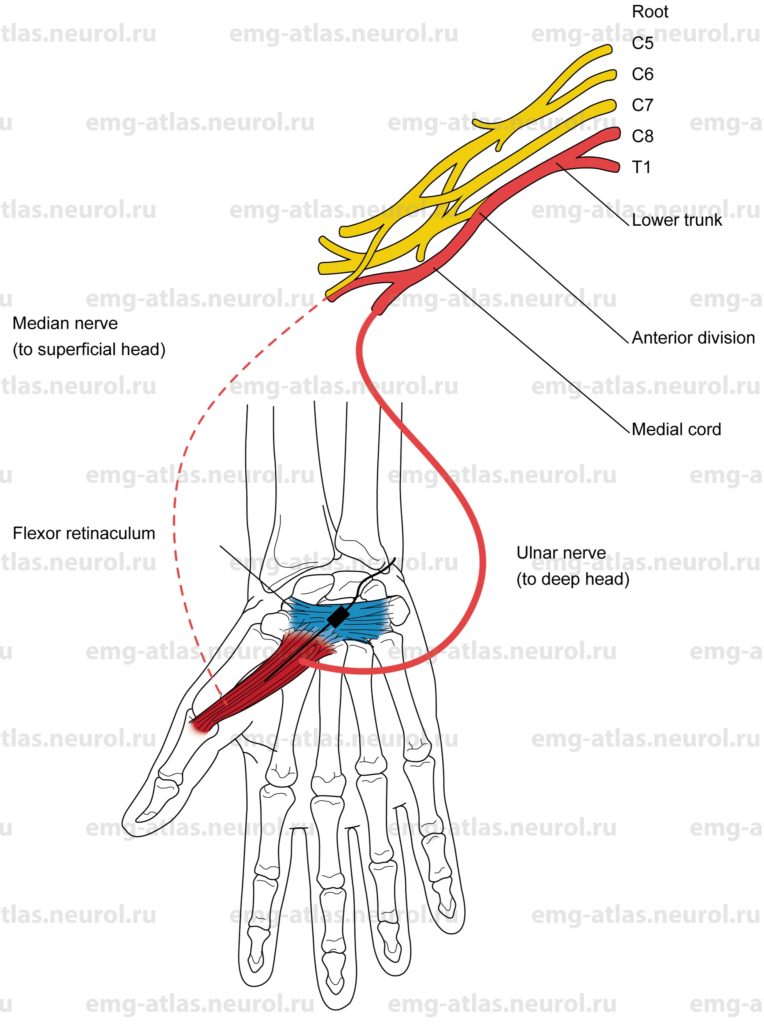
Flexor Pollicis Brevis
Innervation
Superficial head: Innervation is via the median nerve, medial cord, lower trunk, and roots C8, T1.
Deep head: Innervation is via the ulnar nerve, medial cord, lower trunk, and roots C8, T1.
Origin
The superficial head of the flexor pollicis brevis originates in the flexor retinaculum and trapezium.
The deep head of the flexor pollicis brevis originates in the ulnar aspect of the first metacarpal.
Insertion
Superficial head: Insertion is at the radial aspect of the base of the proximal phalanx of the thumb.
Deep head: Insertion is at the ulnar aspect of the base of the proximal phalanx of the thumb.
Activation Maneuver
Flexion of the metacarpophalangeal joint of the thumb activates the muscle.
EMG Needle Insertion
Superficial head: Insert the needle obliquely to a depth of 0.5-1 cm at the midpoint of a line drawn between the metacarpophalangeal joint and the pisiform.
Assess abnormal EMG activity by directing the needle distally along the muscle.
Deep head: The procedure is the same as that for the superficial head except that the needle is inserted to a depth of 1-2 cm.
Pitfalls
If the needle is inserted too deeply, it may penetrate the opponens pollicis, which is innervated by the median nerve; if it is inserted even deeper, it may penetrate the adductor pollicis, which receives innervation from the ulnar nerve.
If the needle is inserted too laterally, it will be in the abductor pollicis brevis, which receives innervation from the median nerve.
Clinical Comments
Examination of the flexor pollicis brevis is rarely of benefit in a routine EMG needle evaluation (in general, muscles that receive dual innervation should be avoided).
The superficial head will show neurogenic changes in lesions of the median nerve.
The deep head will show neurogenic changes in lesions of the ulnar nerve.
In C8, T1, radiculopathy, needle examination will show neurogenic changes if root pathology has resulted in axonal loss in motor fibers (i.e., in moderate to severe radiculopathy).
In Klumpke’s palsy (C8, T1, root avulsion), needle examination will show neurogenic changes.
Anatomical Illustrations
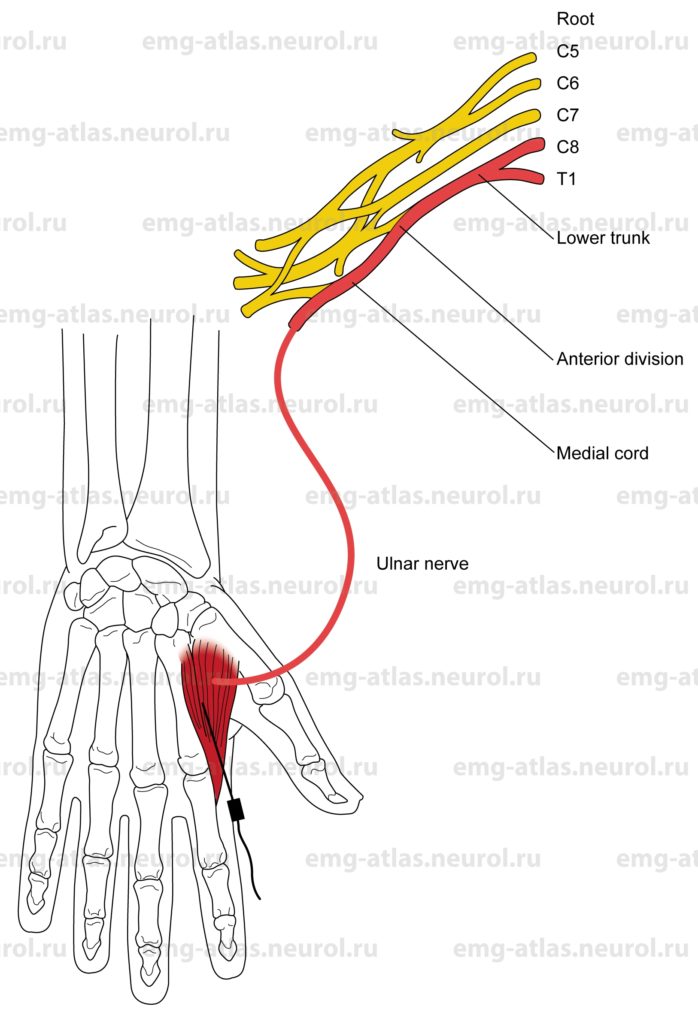
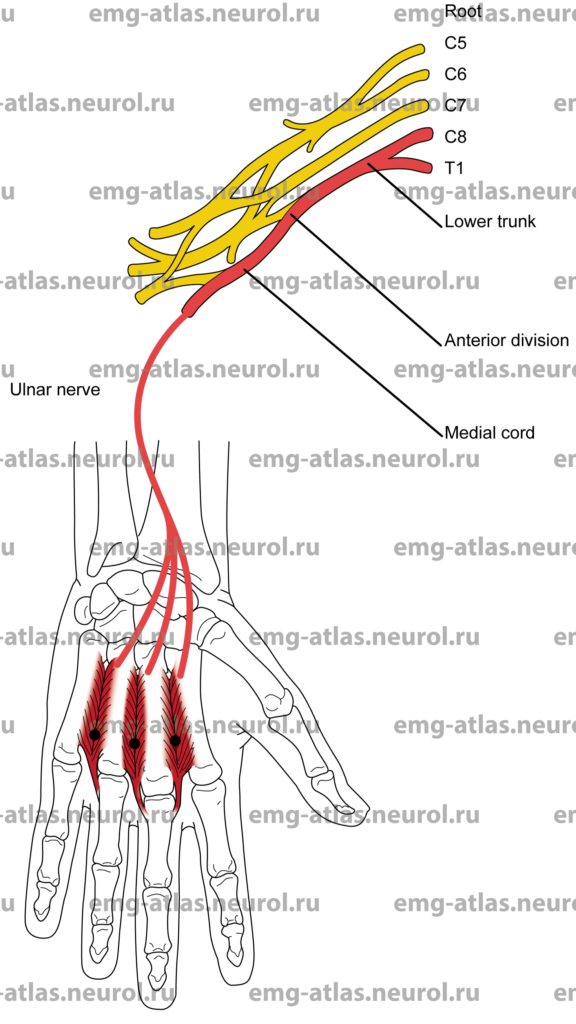
First Dorsal Interosseous
Innervation
Innervation is via the ulnar nerve, medial cord, lower trunk, and roots C8, T1.
Origin
The first dorsal interosseous originates at the ulnar border of the first metacarpal bone (outer head) and the radial border of the second metacarpal bone (inner head).
Insertion
Insertion is at the radial aspect of the base of the proximal phalanx of the index finger.
Activation Maneuver
Abduction (radial deviation) of the index finger activates the muscle.
EMG Needle Insertion
Insert the needle obliquely just proximal to the second metacarpophalangeal joint, and direct it rostrally along the muscle belly.
Pitfalls
There are no pitfalls. If the needle is inserted too deeply, it will still be in C8, T1, muscles innervated by the ulnar nerve.
Clinical Comments
In ulnar neuropathy at the wrist (Guyon’s canal), needle examination may show neurogenic changes when compression produces axonal loss (i.e., in moderate to severe entrapment).
In ulnar neuropathy at the elbow (cubital tunnel, retrocondylar groove), needle examination may show neurogenic changes when compression produces axonal loss.
In C8, T1, radiculopathy, needle examination may show neurogenic changes when root pathology produces axonal loss (i.e., in moderate to severe radiculopathy).
In Klumpke’s palsy (C8, T, root avulsion), needle examination will show neurogenic changes.
Anatomical Illustrations
2nd, 3rd, 4th Dorsal Interossei
Innervation
Innervation is via the ulnar nerve, medial cord, lower trunk, and roots C8, T1.
Origin
The second dorsal interosseous originates at the radial border of the third metacarpal bone and the ulnar border of the second metacarpal bone.
The third and fourth dorsal interossei originate at the ulnar border of the third and fourth metacarpal bones and the radial border of the fourth and fifth metacarpal bones, respectively.
Insertion
Second: Insertion is at the radial aspect of the base of the proximal phalanx of the third digit.
Third and fourth: Insertion is at the ulnar aspect of the base of the proximal phalanx of the third and fourth digit, respectively.
Activation Maneuver
Second: Abduction (radial deviation) of the third digit activates the muscle.
Third and fourth: Adduction (ulnar deviation) of the third and fourth digit, respectively, activates the muscle.
EMG Needle Insertion
Second: Insert the needle just radial to the third metacarpal bone.
Third and fourth: Insert the needle just ulnar to the third and fourth metacarpal bones, respectively.
Pitfalls
There are no pitfalls. If the needle is inserted too deeply, it will still be in C8, T1, muscles innervated by the ulnar nerve.
Clinical Comments
The interossei are occasionally doubled in one or more spaces, or they may be absent in one or more spaces.
There may be variable innervation to these muscles from the median nerve.
Examination of the interossei causes pain and is rarely of benefit in a routine EMG needle evaluation.
In ulnar neuropathy at the wrist (Guyon’s canal), needle examination may show neurogenic changes when compression produces axonal loss (i.e., in moderate to severe entrapment).
In ulnar neuropathy at the elbow (cubital tunnel, retrocondylar groove), needle examination may show neurogenic changes when compression produces axonal loss.
In C8, T1, radiculopathy, needle examination may show neurogenic changes when root pathology produces axonal loss (i.e., in moderate to severe radiculopathy).
In Klumpke’s palsy (C8, T1, root avulsion), needle examination will show neurogenic changes.
Anatomical Illustrations
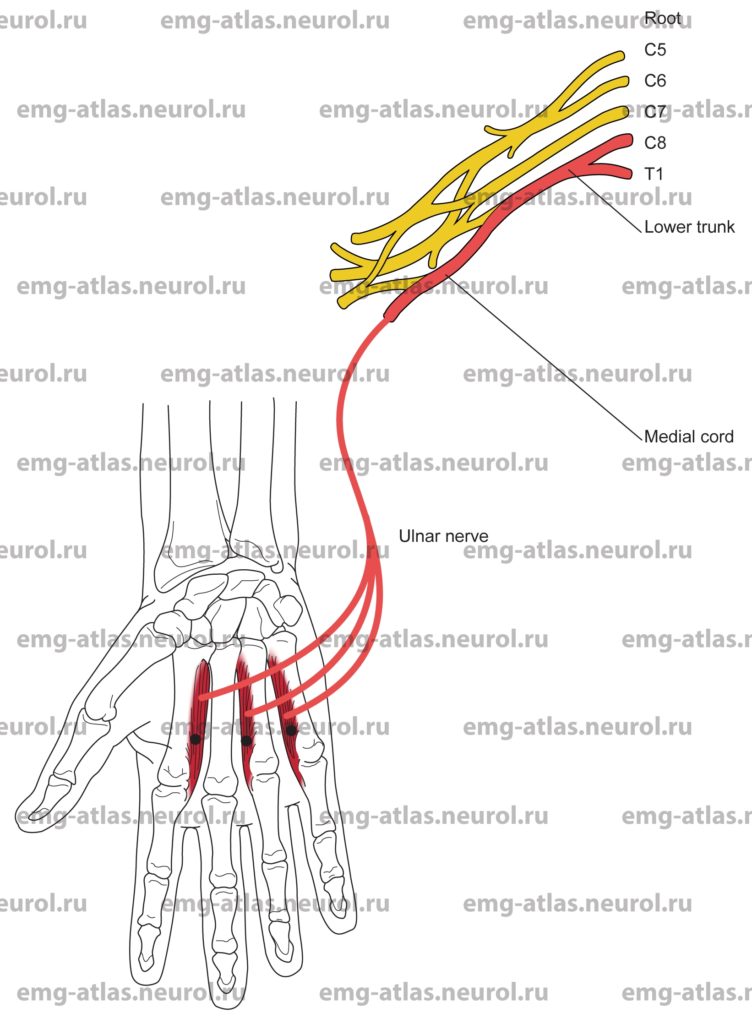
Palmar Interossei
Innervation
Innervation is via the ulnar nerve, medial cord, lower trunk, and roots C8, T1.
Origin
The first palmar interosseous originates at ulnar aspect of the second metacarpal bone.
The second and third palmar interossei originate at the radial aspect of the fourth and fifth metacarpal bones, respectively.
Insertion
First palmar: Insertion is at the ulnar side of the proximal phalanx of the second digit.
Second and third palmar: Insertion is at the radial side of the proximal phalanges of the fourth and fifth digits, respectively.
Activation Maneuver
The palmar interossei adduct the fingers to an imaginary line drawn longitudinally through the center of the third digit middle finger). The first palmar performs ulnar deviation of the second digit; the second and third palmars perform radial deviation of the fourth and fifth digits, respectively.
EMG Needle Insertion
First palmar: Insert the needle just ulnar to the second metacarpal bone.
Second and third palmars: Insert the needle just radial to the fourth and fifth metacarpal bones, respectively.
Pitfalls
There are no pitfalls. If the needle is inserted too deeply, it will still be in C8, T1, muscles innervated by the ulnar nerve.
Clinical Comments
The interossei are occasionally doubled in one or more spaces, or they may be absent in one or more spaces.
There may be variable innervation to these muscles from the median nerve.
Examination of the palmar interossei causes pain and is rarely of benefit in a routine EMG needle evaluation.
In ulnar neuropathy at the wrist (Guyon’s canal), needle examination may show neurogenic changes when compression produces axonal loss (i.e., in moderate to severe entrapment).
In ulnar neuropathy at the elbow (cubital tunnel, retrocondylar groove), needle examination may show neurogenic changes when compression produces axonal loss.
In C8, T1, radiculopathy, needle examination may show neurogenic changes when root pathology produces axonal loss (i.e., in moderate to severe radiculopathy).
In Klumpke’s palsy (C8, T1, root avulsion), needle examination will show neurogenic changes.
Anatomical Illustrations
3rd, 4th Lumbricals
Innervation
Innervation is via the ulnar nerve, medial cord, lower trunk, and roots C8, T1.
Origin
The third and fourth lumbricals originate at the radial aspect of the tendon sheath of the flexor digitorum profundus.
Insertion
Insertion is at the radial lateral band of the dorsal digital expansion (tendinous expansion of the extensor digitorum communis).
Activation Maneuver
Extension of the finger at the proximal interphalangeal joint with the metacarpophalangeal joint extended and fixed activates the muscles.
EMG Needle Insertion
Insert the needle just proximal to the metacarpophalangeal joint and radial to the flexor tendon.
Pitfalls
There are no pitfalls. All muscles surrounding the third and fourth lumbricals receive innervation from the ulnar nerve.
Clinical Comments
Examination of the third and fourth lumbricals causes pain and is rarely of benefit in a routine EMG needle evaluation.
In ulnar neuropathy at the wrist (Guyon’s canal), needle examination may show neurogenic changes when compression produces axonal loss (i.e., in moderate to severe entrapment.
In ulnar neuropathy at the elbow (cubital tunnel, retrocondylar groove), needle examination may show neurogenic changes when compression produces axonal loss.
In C8, T1, radiculopathy, needle examination may show neurogenic changes when root pathology produces axonal loss (i.e., in moderate to severe radiculopathy).
In Klumpke’s palsy (C8, T1, root avulsion), needle examination will show neurogenic changes.
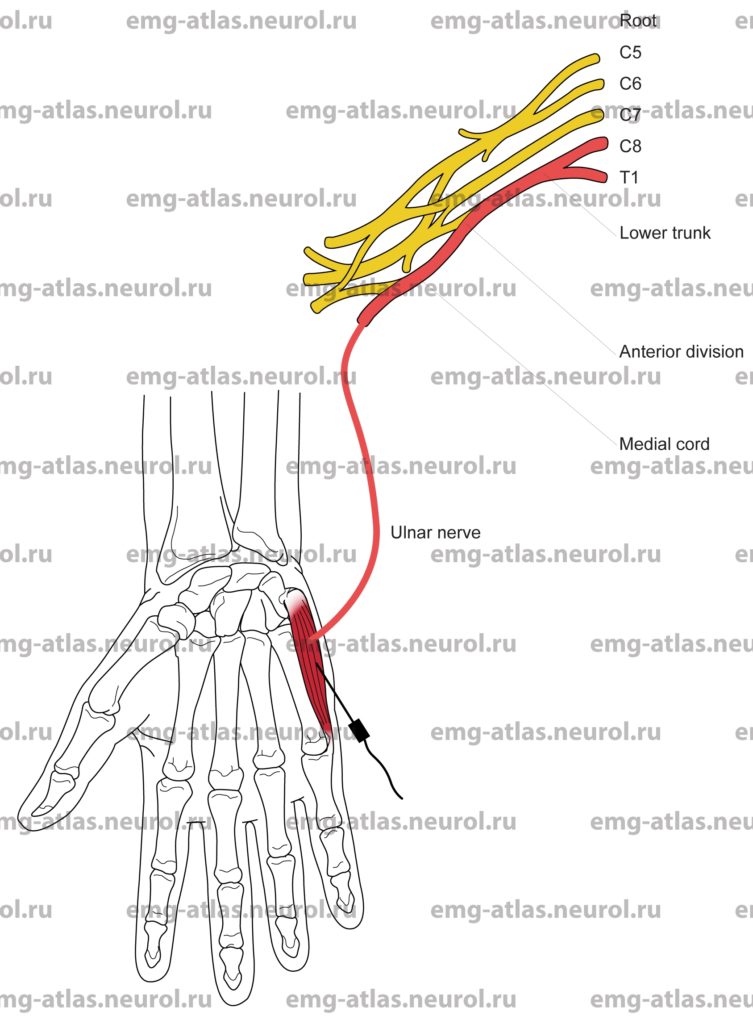
Anatomical Illustrations
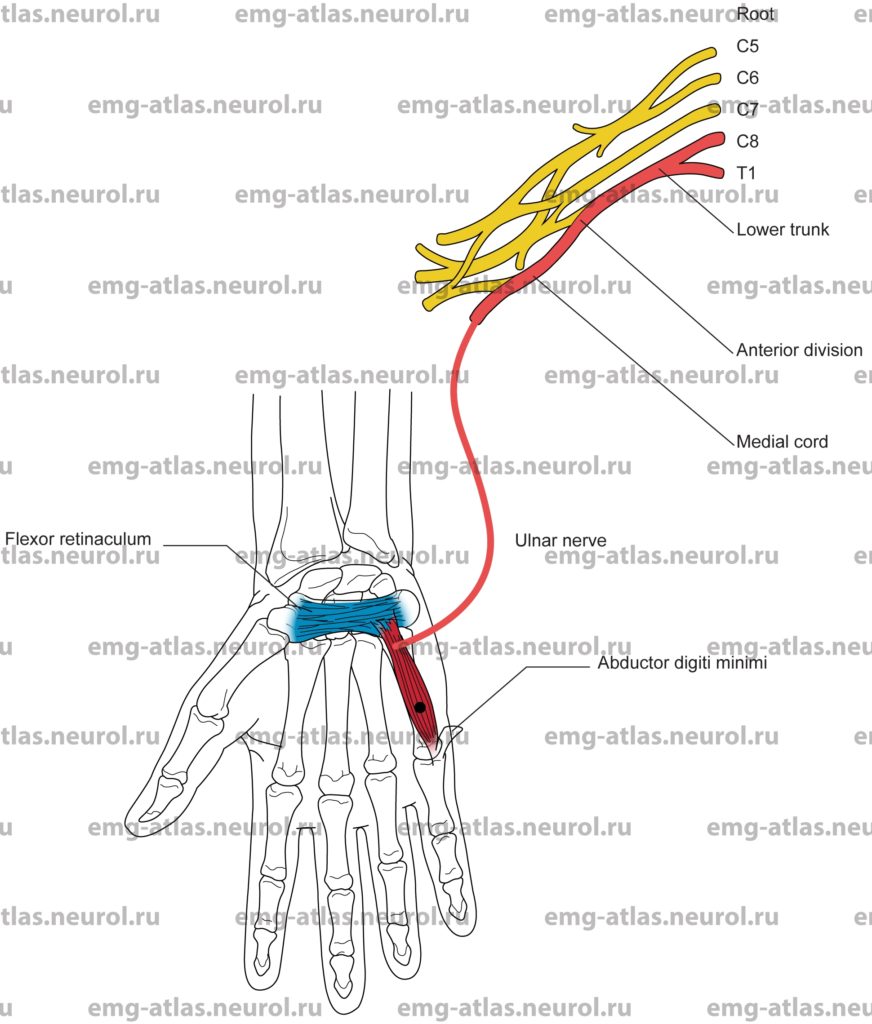
Abductor Digiti Minimi
Innervation
Innervation is via the ulnar nerve, medial cord, lower trunk, and roots C8, T1.
Origin
The abductor digit minimi originate at the pisiform bone.
Insertion
Insertion is at the medial side of the base of the proximal phalanx of the little finger.
Activation Maneuver
Abduction of the little finger activates the muscles.
EMG Needle Insertion
Insert the needle obliquely at the midpoint between the fifth metacarpophalangeal joint (metacarpophalangeal crease) and the ulnar aspect of the pisiform (distal wrist crease).
Pitfalls
There are no pitfalls. If the needle is inserted too deeply or laterally, it will still be in C8, T1, muscles innervated by the ulnar nerve.
Clinical Comments
In ulnar neuropathy at the wrist (Guyon’s canal), needle examination may show neurogenic changes when compression produces axonal loss (i.e., in moderate to severe entrapment).
In ulnar neuropathy at the elbow (cubital tunnel, retrocondylar groove), needle examination may show neurogenic changes when compression produces axonal loss.
In C8, T1, radiculopathy, needle examination may show neurogenic changes when root pathology produces axonal loss (i.e., in moderate to severe radiculopathy).
In Klumpke’s palsy (C8, T1, root avulsion), needle examination will show neurogenic changes.
Anatomical Illustrations
Opponens Digiti Minimi
Innervation
Innervation is via the ulnar nerve, medial cord, lower trunk, and roots C8, T1.
Origin
The opponens digiti minimi originate at the flexor retinaculum and the hook of the hamate.
Insertion
Insertion is at the ulnar margin of the fifth metacarpal bone.
Activation Maneuver
Opposition of the little finger to the thumb activates the muscles.
EMG Needle Insertion
Insert the needle at the midpoint between the fifth metacarpophalangeal joint metacarpophalangeal crease) and the pisiform distal wrist crease), just radial to the abductor digiti minimi.
Pitfalls
There are no pitfalls. If the needle is inserted too deeply or laterally, it will still be in C8, T1, muscles innervated by the ulnar nerve.
Clinical Comments
In ulnar neuropathy at the wrist (Guyon’s canal), needle examination may show neurogenic changes when compression produces axonal loss (i.e., in moderate to severe entrapment).
In ulnar neuropathy at the elbow (cubital tunnel, retrocondylar groove), needle examination may show neurogenic changes when compression produces axonal loss.
In C8, T1 radiculopathy, needle examination may show neurogenic changes when root pathology produces axonal loss (i.e., in moderate to severe radiculopathy).
In Klumpke’s palsy (C8, T1, root avulsion), needle examination will show neurogenic changes.
Anatomical Illustrations
Flexor Digiti Minimi
Innervation
Innervation is via the ulnar nerve, medial cord, lower trunk, and roots C8, T1.
Origin
The flexor digiti minimi originate at the hook of the hamate and the flexor retinaculum.
Insertion
Insertion is at the ulnar side of the base of the proximal phalanx of the little finger.
Activation Maneuver
Flexion of the proximal phalanx of the fifth digit activates the muscles.
EMG Needle Insertion
Insert the needle at the midpoint between the fifth metacarpophalangeal joint (metacarpophalangeal crease) and the ulnar aspect of the pisiform (distal wrist crease), just radial to the abductor digiti minimi.
Pitfalls
There are no pitfalls. If the needle is inserted too deeply, it will be in the opponens digiti minimi, which is still innervated by the ulnar nerve.
Clinical Comments
In ulnar neuropathy at the wrist (Guyon’s canal), needle examination may show neurogenic changes when compression produces axonal loss (i.e., in moderate to severe entrapment).
In ulnar neuropathy at the elbow (cubital tunnel, retrocondylar groove), needle examination may show neurogenic changes when compression produces axonal loss.
In C8, T1, radiculopathy, needle examination may show neurogenic changes when root pathology produces axonal loss (i.e., in moderate to severe radiculopathy).
In Klumpke’s palsy (C8, T1, root avulsion), needle examination will show neurogenic changes.
Anatomical Illustrations
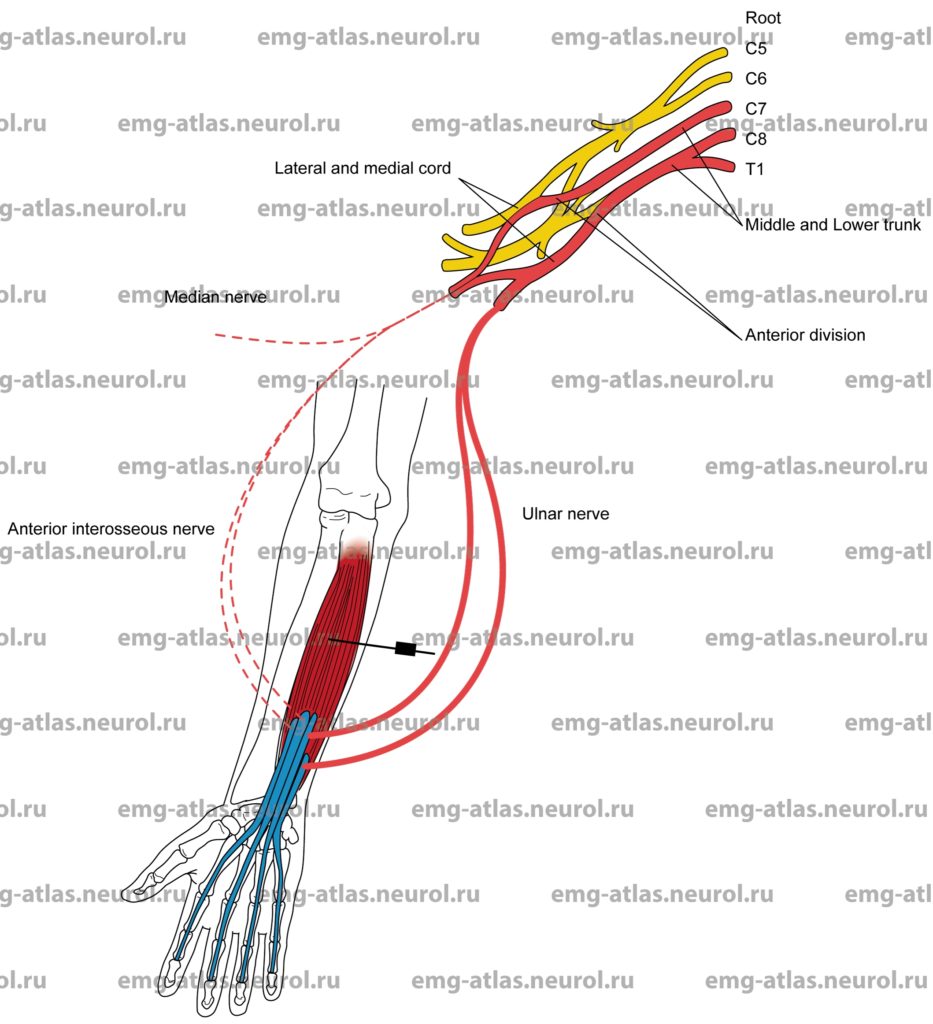
Flexor Digitorum Profundus Digits 4 and 5
Innervation
Digits four and five: Innervation is via the ulnar nerve, medial cord, lower trunk, and roots C8, T1.
Digits two and three: Innervation is via the anterior interosseous branch, median nerve, lateral and medial cords, middle and lower trunks, and roots C7, C8.
Origin
The flexor digitorum profundus originates at the volar and medial surfaces of the shaft of the ulna.
Insertion
Insertion is at the volar surfaces of the bases of the distal phalanges of digits 2 through 5.
Activation Maneuver
Flexion of the distal phalanges of digits 4 and 5 activates the muscle.
EMG Needle Insertion
Palpate the shaft of the ulna along the medial forearm. Insert the needle 5-7 cm distal to the olecranon process and 1-1.5 cm medial to the shaft of the ulna.
The ulna-innervated portion lies superficially at a depth of 1-2 cm; the median portion lies deep at a depth of 3-4 cm. Note: The easiest approach to this muscle is for the subject to place the forearm perpendicular to the table with the hand and wrist relaxed. The shaft of the ulna and the adjacent belly of the muscle can easily be palpated (see photograph).
Pitfalls
If the needle is inserted too volary (i.e., toward the palmar surface), it may lie in the flexor carpi ulnaris, which also receives innervation from the ulnar nerve.
Clinical Comments
Needle examination of the superficial portion may show neurogenic changes in axonal loss lesions of the ulnar nerve at the elbow (cubital tunnel or retrocondylar groove).
Needle examination of the deep portion may show neurogenic changes if a lesion of the anterior interosseous nerve produces axonal loss and in axonal loss lesions of the median nerve at the elbow (pronator teres syndrome) or above the elbow (ligament of Struther’s syndrome).
In C8, T1, radiculopathy, the needle examination may show neurogenic changes when root pathology has resulted in axonal loss (i.e., in moderate to severe radiculopathy).
In Klumpke’s palsy (C8, T1, root avulsion), needle examination will show neurogenic changes.
Anatomical Illustrations
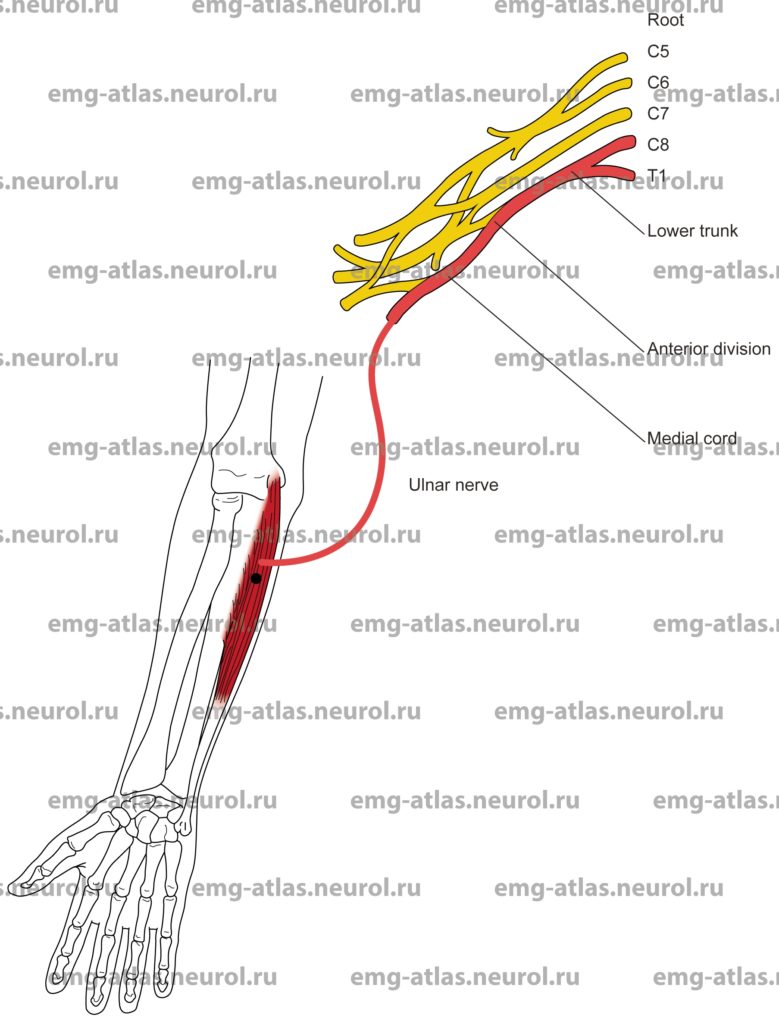
Flexor Carpi Ulnaris
Innervation
Innervation is via the ulnar nerve, medial cord, lower trunk, and roots C8, T1.
Origin
The flexor carpi ulnaris arises by two heads.
One head is from the medial epicondyle of the humerus, and the other head is from the olecranon process and the upper two-thirds of the posterior border of the ulna.
Insertion
Insertion is at the pisiform, hamate, and fifth metacarpal bones.
Activation Maneuver
Flexion at the wrist with ulnar deviation activates the muscles.
EMG Needle Insertion
Insert the needle 5-8 cm distal to the medial epicondyle along a line connecting the medial epicondyle and pisiform bone.
Pitfalls
If the needle is inserted too laterally (radially), it may be in the palmaris longus or the flexor carpi radialis, both muscles innervated by the median nerve.
If the needle is inserted too deeply, it may be in the flexor digitorum superficialis (supplied by median nerve), or, if still deeper, it may penetrate the flexor digitorum profundus (supplied by median and ulnar nerves).
Clinical Comments
The two heads are connected by a tendinous arch that forms the cubital tunnel 1-2 cm distal to the medial epicondyle, through which passes the ulnar nerve.
Entrapment at this site produces ulnar neuropathy at the elbow (cubital tunnel).
Needle examination of this muscle is usually normal in cubital tunnel entrapment. It may also be normal in ulnar neuropathy due to compression at the retrocondylar groove.
In C8, T1, radiculopathy, needle examination may show neurogenic changes when root pathology produces axonal loss (i.e., in moderate to severe radiculopathy).
In Klumpke’s palsy (C8, T1, root avulsion), needle examination will show neurogenic changes.