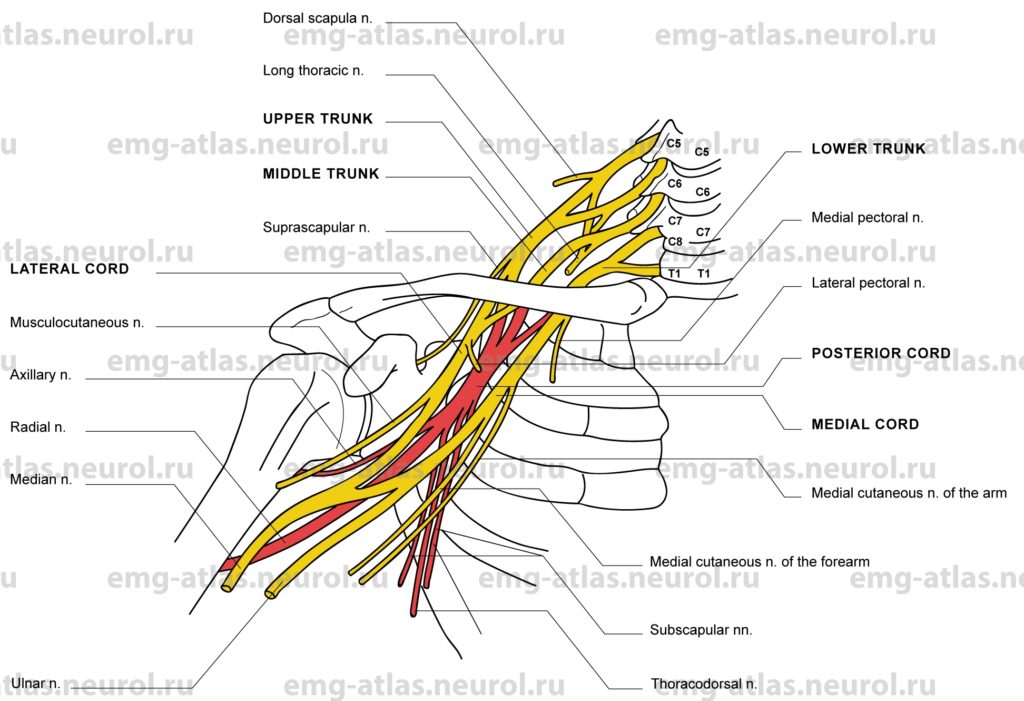
The brachial plexus is formed by the union of the fifth, sixth, seventh, and eighth cervical ventral rami and the first thoracic ventral ramus (Gray’s Anatomy, 1995). Contributions to the plexus from C4 and T2 vary. In a prefixed plexus, the contribution from C4 is large and the branch from T, is reduced. In a postfixed plexus, the contribution from T2 is large and the branch from C5 is reduced. In the most common arrangement, the C5 and C6 rami unite at the lateral border of the scalenus medius to form the upper trunk, C7 gives rise to the middle trunk, and C8 and T, join behind the scalenus anterior as the lower trunk. The three trunks descend laterally; at the level of the clavicle each trunk bifurcates into anterior and posterior divisions. The anterior divisions of the upper and middle trunks form the lateral cord, lateral to the axillary artery. The anterior division of the lower trunk emerges medial to the axillary artery to form the medial cord, which may also receive a branch from the C7 ramus. Posterior divisions of all three trunks form the posterior cord, posterior to the axillary artery.
Brachial plexus lesions may involve the entire plexus or be confined to a particular part of it; the degree of nerve injury is seldom uniform. Acute lesions of the brachial plexus may be due to open or closed injury. In open injuries, wounding is commonly due to gun shot or sharp penetrating objects and involves the more superficial part of the plexus. Wounding involving the lower plexus is more likely to be fatal because of simultaneous damage to the lung and great vessels at the root of the neck (Sunderland, 1968). In closed injuries the causative agent is commonly traction or compression of the plexus. Neuralgic amyotrophy, also known as idiopathic brachial plexopathy, Parsonage-Turner syndrome, shoulder girdle neuritis, or acute brachial neuropathy, ranks first in incidence among nontraumatic conditions (Beghi et al., 1985), and most commonly affects the upper plexus and shoulder girdle muscles (Subramony, 1988).
Upper Trunk Lesion
Etiology
Neuralgic amyotrophy is the most common nontraumatic condition and usually affects the upper plexus and shoulder girdle muscles.
Trauma, including stab or gunshot wounds.
Stretch injuries occur when the neck and shoulder are violently forced apart, when a blow or heavy weight depresses the shoulder, or when an adducted limb is forced violently downward (Sunderland, 1968). Stretch injuries include traction injury during difficult delivery (birth palsy), “rucksack” or “pack palsy” due to lifting a heavy backpack, and the football injury known as a “stinger” (Kimura, 1989).
General Comments
Stretch injuries to the upper trunk may be combined with C5, C6 root avulsion (Erb’s palsy).
Clinical Features
The distribution of weakness is similar to that of Erb’s palsy, with involvement of the shoulder and upper arm and sparing of hand function.
There is gross wasting of shoulder girdle muscles with a complete inability to abduct or externally rotate the arm and marked weakness of elbow flexion and radial wrist extension.
Numbness occurs over the lateral aspects of the arm, forearm, and hand.
The biceps stretch reflex is absent or reduced.
Electrodiagnostic Strategy
Use nerve conduction studies to confirm a lesion of the upper trunk (low amplitude or unelicitable sensory responses from superficial radial, lateral cutaneous nerve of forearm and median nerve recording from thumb or index finger; low amplitude or unelicitable motor responses from biceps and deltoid). In a predominantly demyelinating lesion, routine nerve conduction studies may be normal; search for local demyelinating block or slowing of conduction across the site of injury. Note: Sensory responses are normal in radiculopathies because the lesion is proximal to the dorsal root ganglion (preganglionic lesion) and the cell bodies in the ganglion maintain viability of the peripheral sensory fiber.
Demonstrate neurogenic electromyography (EMG) needle examination (i.e., spontaneous activity, abnormal motor unit potentials, abnormal recruitment) in muscles supplied by the upper trunk
Use needle EMG to exclude C5, C6 radiculopathies. Radiculopathies may produce neurogenic findings in paraspinal muscles as well as limb muscles; plexopathies never do so because the plexus is formed by ventral rami, whereas paraspinal muscles are innervated by posterior rami (Wilbourn, 1985).
Middle Trunk Lesion
Etiology
Neuralgic amyotrophy is a nontraumatic cause.
Isolated injury to the middle trunk is rare.
With lateral traction on the arm, the middle trunk may be the first to be injured (Sunderland, 1968).
General Comments
The middle trunk occupies a position between upper and lowertrunks, being at times damaged with either the upper plexus or the lower plexus.
Clinical Features
Weakness occurs in the general territory of the radial nerve, with partial involvement of the triceps and other C7 -innervated muscles and sparing of brachioradialis.
Numbness or loss of sensation occurs in the middle finger and sometimes the index finger.
The triceps stretch reflex may be reduced.
Electrodiagnostic Strategy
Nerve conduction studies may suggest a lesion of the middle trunk (low amplitude or unelicitable sensory responses from median nerve-innervated middle finger and possibly index finger; the remaining studies are normal). In a demyelinating lesion, routine nerve conduction studies may be normal; search for local demyelinating block or slowing of conduction across the site of injury. Note: Sensory responses are normal in a C7 radiculopathy because the lesion is proximal to the dorsal root ganglion (preganglionic lesion) and the cell bodies in the ganglion maintain viability of the peripheral sensory fibers.
Demonstrate neurogenic EMG needle examination (i.e., spontaneous activity, abnormal motor unit potentials, abnormal recruitment) in muscles supplied by the middle trunk.
Use needle EMG to exclude C7 radiculopathy. Radiculopathies may produce neurogenic EMG in paraspinal muscles as well as limb muscles; plexopathies never do so because the plexus is formed by ventral rami, whereas paraspinal muscles are innervated by posterior rami (Wilbourn, 1985).
Lower Trunk Lesion
Etiology
Metastasis (lymph node infiltration in axilla) or direct invasion (Pancoast’s tumor in apex of lung) can cause a lower trunk lesion.
Neuralgic amyotrophy is a nontraumatic cause.
Neurogenic thoracic outlet syndrome (TOS) is a rare cause.
Traumatic causes include stab wounds and bullet wounds.
Traction applied to the fully abducted arm (i.e., subject jerked upward by the outstretched arm) can cause a lower trunk lesion.
General Comments
True neurogenic TOS is rare (1 per 1,000,000) and results from lowertrunk fibers being stretched over a fibrous band extending from the first rib to the C7 transverse process or a rudimentary cervical rib (Wilbourn, 1988).
When traction is applied to the fully abducted arm, it is the lower roots and trunk of the plexus that suffer most (Sunderland, 1968).
Stretch injuries to the lowertrunk may be combined with C8, T, root avulsion (Klumpke’s palsy).
Clinical Features
The distribution of weakness is similar to that of Klumpke’s palsy, with involvement of all intrinsic hand muscles and sparing of shoulder and upper arm muscles.
In addition to intrinsic hand muscles, finger flexors and extensors in the forearm are weak
Numbness or loss of sensation occurs in the medial aspect of the arm, medial forearm, and medial hand, including fourth and fifth digits.
Electrodiagnostic Strategy
Use nerve conduction studies to localize a lesion to the lowertrunk or medial cord (low amplitude or unelicitable sensory responses from little finger and medial cutaneous nerve of forearm; low amplitude or unelicitable motor responses from median and ulnar hand muscles). In a demyelinating lesion, special nerve conduction studies may be needed to demonstrate demyelinating block or slowing of conduction across the site of injury. Note: Sensory responses are normal in radiculopathies because the lesion is proximal to the dorsal root ganglion.
Demonstrate neurogenic EMG needle examination (i.e., spontaneous activity, abnormal motor unit potentials, abnormal recruitment) in muscles supplied by the lower trunk exclude C8, T1 radiculopathies by needle EMG. Radiculopathies may produce neurogenic EMG in paraspinal muscles as well as limb muscles; plexopathies never do so because the plexus is formed by ventral rami, whereas paraspinal muscles are innervated by posterior rami (Wilbourn, 1985).
Cord Lesions
General Comments
The consequences of lesions affecting the lateral, medial, or posterior cords of the brachial plexus may be determined by combining the effects following injury to the individual nerves that originate from the respective cords (Sunderiand, 1968).