Anterior and posterior roots form the spinal nerves that exit through the intervertebral foramina. There are 31 spinal nerves on each side: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral and 1 coccygeal nerve. Immediately after passing through the foramina, the spinal nerves branch into two divisions, the anterior and posterior rami.
The anterior rami form the cervical, brachial, lumbar and sacral plexuses, which in turn give rise to the peripheral nerves in the neck and upper and lower limbs. The anterior rami of the thoracic spinal nerves become the 12 pairs of intercostal nerves that supply the intercostal and abdominal muscles.
The posterior rami supply the paraspinal muscles in the cervical, thoracic and lumbosacral regions. These muscles extend the head, neck, trunk, and pelvis. Because the posterior rami branch off the spinal nerve just distal to the intervertebral foremen, needle electromyogram (EMG) abnormalities in paraspinal muscles usually imply axonal loss at the root level (i.e., radiculopathy). However, radiculopathy causes EMG abnormalities in paraspinal muscles only after structural damage or axonal loss has occurred. Hence, the EMG may be normal when a compressing lesion irritates the root without causing axonal loss (Kimura, 1989). Moreover, the EMG in paraspinal muscles may be normal in the early stages of disease. Signs of denervation may not appear in paraspinal muscles for several days and in limb muscles for several weeks after severe root injury. Lesions limited to the plexuses or peripheral nerves do not produce EMG abnormalities in paraspinal muscles.
Anatomical Illustrations
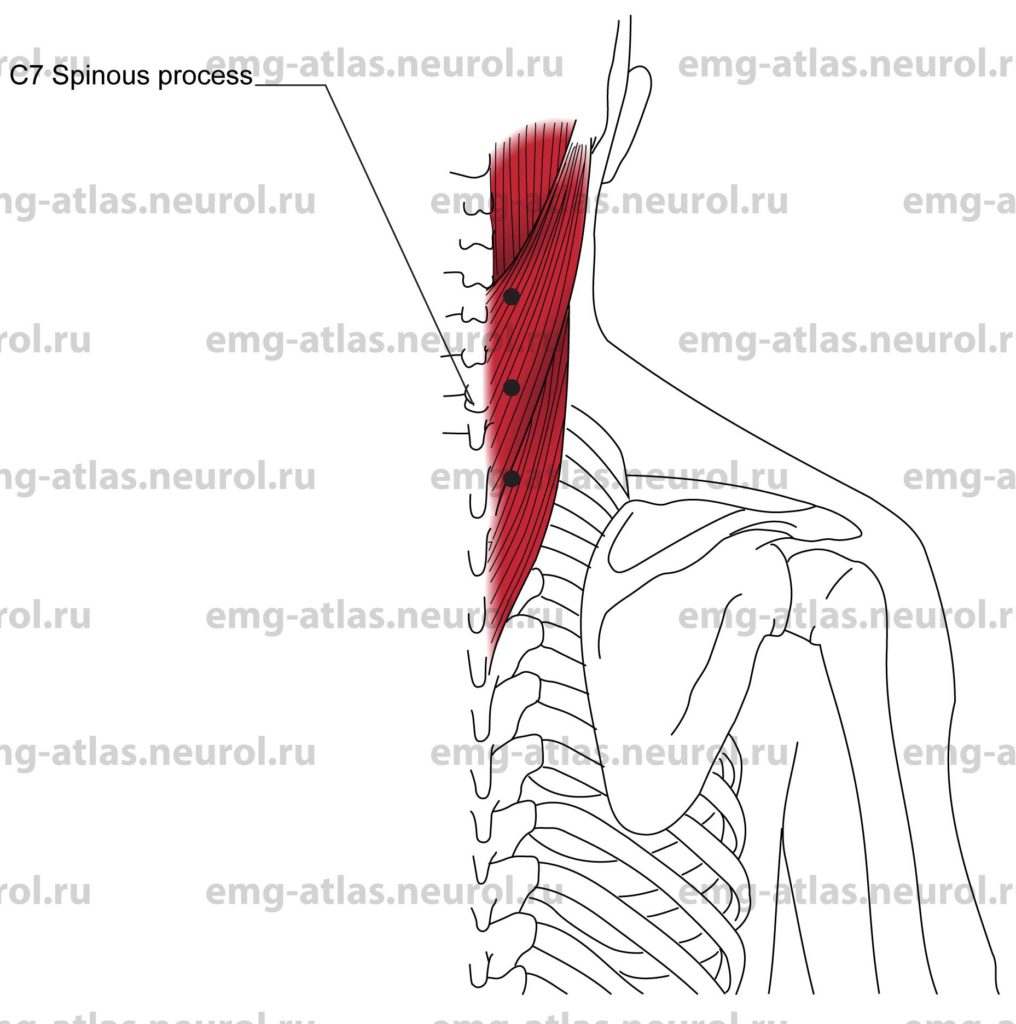
Cervical Paraspinal
Innervation
Innervation is via the posterior primary rami of the cervical spinal nerves at the respective segmental levels.
Origin
The muscles of the paraspinal region are numerous and situated in superficial to deep layers (Gray’s Anatomy, 1977). The most superficial muscles include the upper trapezius, levator scapulae, and rhomboids, with the splenius capitus and erector spinae (longissimus dorsi, transversalis colli) intermediate in depth. The deeper muscles include the multifidus, supraspinalis, interspinales, rectus capitis, and obliquus capitis, which lie deep against the vertebrae. The close proximity and overlap of the intermediate and deeper muscles makes it impossible to isolate them individually by needle examination. In general, however, the deeper muscles are shorter and receive a more discrete nerve supply from the corresponding posterior rami, whereas the more intermediate muscles are longer and receive a more overlapping nerve supply.
Insertion
It is not possible to describe all of the attachments of the muscles of the paraspinal region.
Patient Position
To achieve complete relaxation, the patient lies in the prone position with pillows underneath the chest and the forehead resting against the examining table. If full relaxation cannot be obtained, ask the patient to gently press the forehead against the table (this will cause reciprocal inhibition of the cervical paraspinal muscles).
Activation Maneuver
Ask the patient to extend the head.
EMG Needle Insertion
Identify the C7 spinous process (the most prominent process), and count the remaining spinous processes to determine the level of the spine to be examined. Insert the needle perpendicular to the skin, or slightly upward, about 2 cm lateral to the spinous process of the desired level. The needle should encounter the lamina of the vertebra to assess the deep muscles.
Pitfalls
If the needle is too superficial, it may be in the trapezius, levator scapulae, or rhomboids.
In about 20% of thin subjects, lung tissue extends above the clavicle with a distance from skin surface to lung tissue of about 3.3 cm (Honet et al., 1986). Rarely, pneumothorax can occur following needle examination of paraspinal muscles (Honet et al., 1986). One can minimize the risk of pneumothorax by inserting the needle close to the midline, particularly when studying the lower cervical or thoracic paraspinal muscles.
The innervation to the cervical paraspinal muscles may extend one or two segments below a particular, level. This anatomical variability makes it difficult to determine the precise localization in cases of radiculopathy.
Anatomical Illustrations
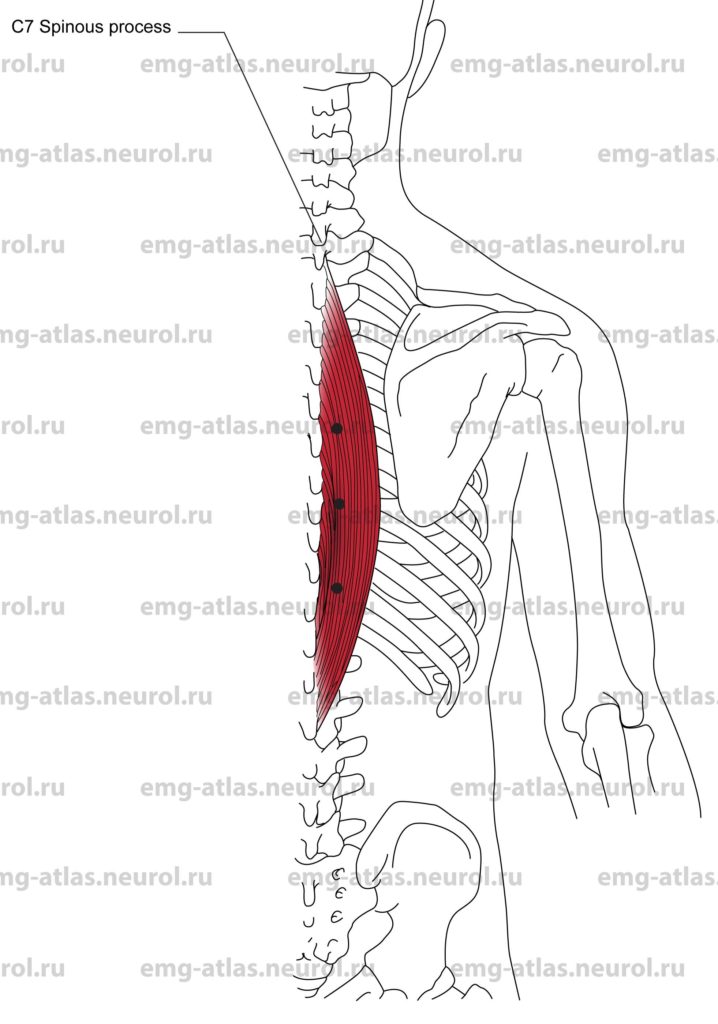
Thoracic Paraspinal
Innervation
Innervation is via the posterior primary rami of the thoracic spinal nerves at the respective segmental levels.
Origin
The muscles of the thoracic paraspinal region are numerous and situated in superficial to deep layers (Gray’s Anatomy, 1977). Superficial muscles include the middle and lower trapezius and latissimus dorsi, with the erector spinae (longissimus dorsi, transversalis colli, spinalis dorsi) intermediate in depth. The deeper muscles include the multifidus, rotatores, interspinales, and semispinalis, which lie deep against the vertebrae. The close proximity and overlap of the intermediate and deeper muscles makes it impossible to isolate them individually by needle examination. In general, however, the deeper muscles are shorter and receive a more discrete nerve supply from the corresponding posterior rami, whereas the more intermediate muscles are longer and receive a more overlapping nerve supply.
Insertion
It is not possible to describe all of the attachments of the muscles of the paraspinal region.
Patient Position
The patient lies in the prone position with pillows underneath the chest and the forehead resting against the examining table. Alternatively, the patient may be flat or in the side-lying fetal position.
Activation Maneuver
Ask the patient to gently arch the back.
EMG Needle Insertion
Identify the C, spinous process (the most prominent process), and count down the remaining spinous processes to determine the level of the spine to be examined. Insert the needle perpendicular to the skin, about 2 cm lateral to the spinous process of the desired level. The needle should encounter the lamina of the vertebra to assess the deep muscles.
Pitfalls
If the needle is too superficial, it may be in the trapezius or latissimus dorsi.
Rarely, pneumothorax can occur following needle examination of paraspinal muscles (Honet et al., 1986). One can minimize the risk of pneumothorax by inserting the needle close to the midline.
Clinical Comments
Documentation of EMG abnormalities in thoracic paraspinal muscles suggests axonal loss affecting the spinal nerve proximal to its bifurcation into posterior and anterior rami (i.e., at the root level).
Some systemic conditions, most notably polymyositis, may affect the paraspinal muscles preferentially and sometimes exclusively (Kimura, 1989; Petrella et al., 1997).
Anatomical Illustrations
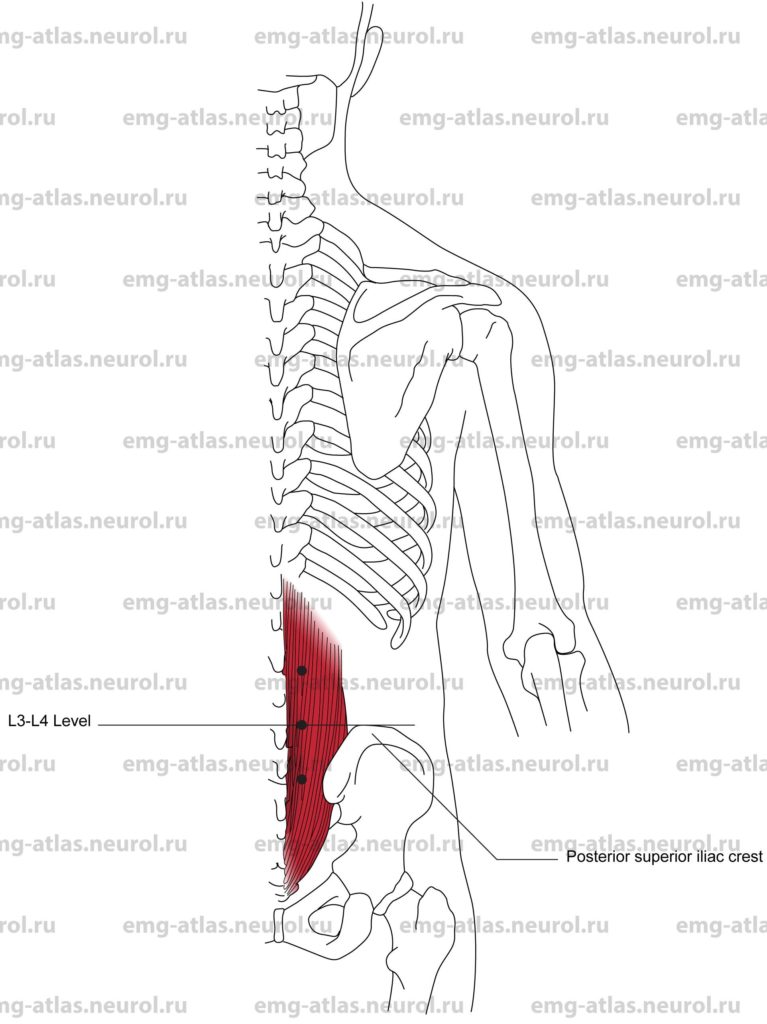
Lumbosacral Paraspinal
Innervation
Innervation is via the posterior primary rami of the lumbar and sacral spinal nerves at the respective levels.
Origin
The muscles of the paraspinal region are numerous and situated in superficial to deep layers (Gray’s Anatomy, 1977). Superficial muscles include the latissimus dorsi, with the erector spinae (longissimus dorsi, spinalis dorsi) intermediate in depth. The deeper muscles include the multifidus and interspinales, which lie deep against the vertebrae. The close proximity and overlap of these muscles makes it impossible to isolate them individually by needle examination. In general, however, the deeper muscles are shorter and receive a more discrete nerve supply from the corresponding posterior rami, whereas the more superficial muscles are longer and receive a more overlapping nerve supply.
Insertion
It is not possible to describe all of the attachments of the muscles of the paraspinal region.
Patient Position
The patient lies in the prone position with pillows placed underneath the abdomen. Alternatively, the patient may be in the side-lying fetal position. In the latter position, the muscles on the side farthest from the table are generally relaxed.
Activation Maneuver
For the prone position, ask the patient to elevate the whole leg (perform hip extension). For the side-lying fetal position, ask the patient to perform hip extension against resistance by the examiner.
EMG Needle Insertion
Draw an imaginary line connecting the posterior superior iliac crests. This line intersects the lumbar spine at the L3-L4 intervertebral level. Count up or down the spinous processes to determine the paraspinal level to be examined. Insert the needle perpendicular to the skin, about 2 cm lateral to the spinous process of the desired level. The needle should encounter the lamina of the vertebra to assess the deep muscles.
Pitfalls
If the needle is too superficial, it may be in the latissimus dorsi.
To facilitate relaxation of these muscles, instruct the patient to push the small of the back against the examiner’s hands. Clinical Comments
Documentation of EMG abnormalities in lumbosacral paraspinal muscles suggests axonal loss affecting the spinal nerve proximal to its bifurcation into the posterior and anterior rami (i.e., at the root level).
Some systemic conditions, most notably polymyositis, may affect the paraspinal muscles preferentially and sometimes exclusively (Kimura, 1989; Petrella et. al., 1997).