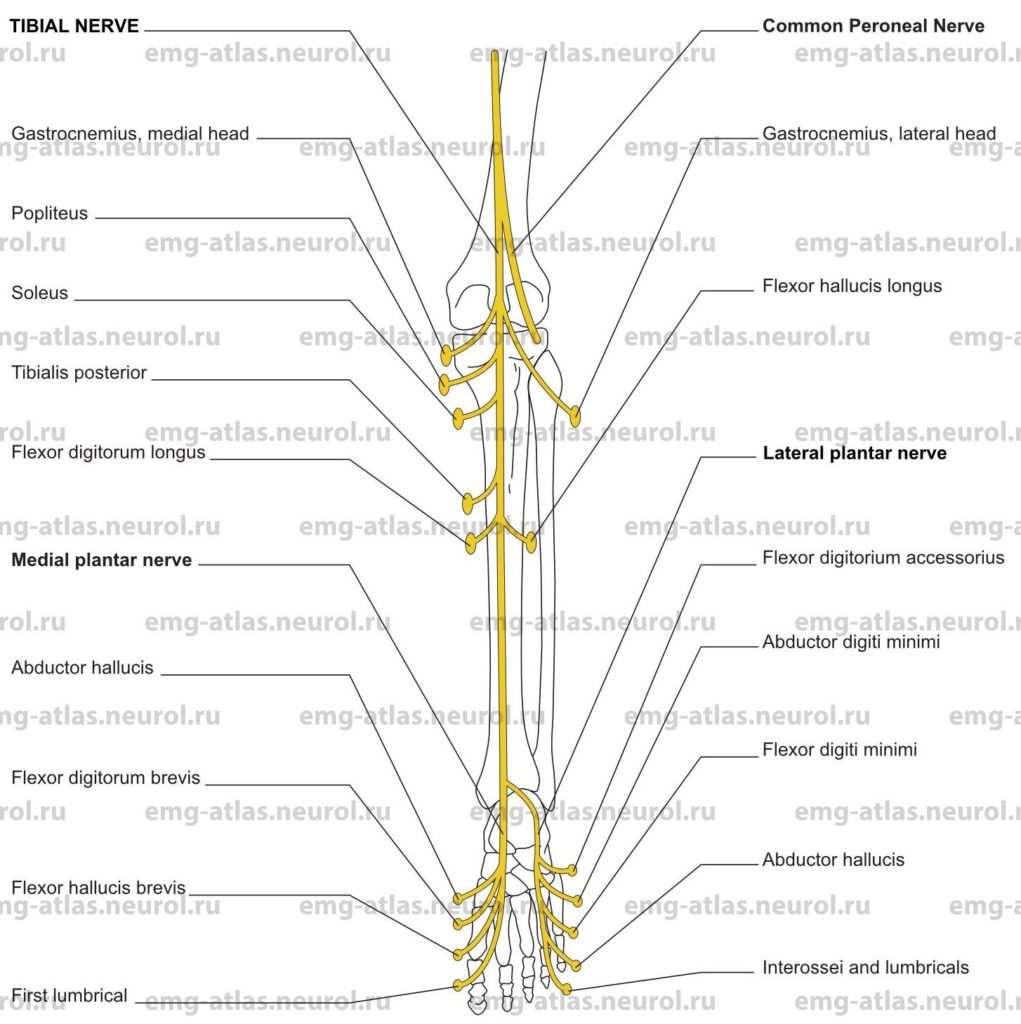
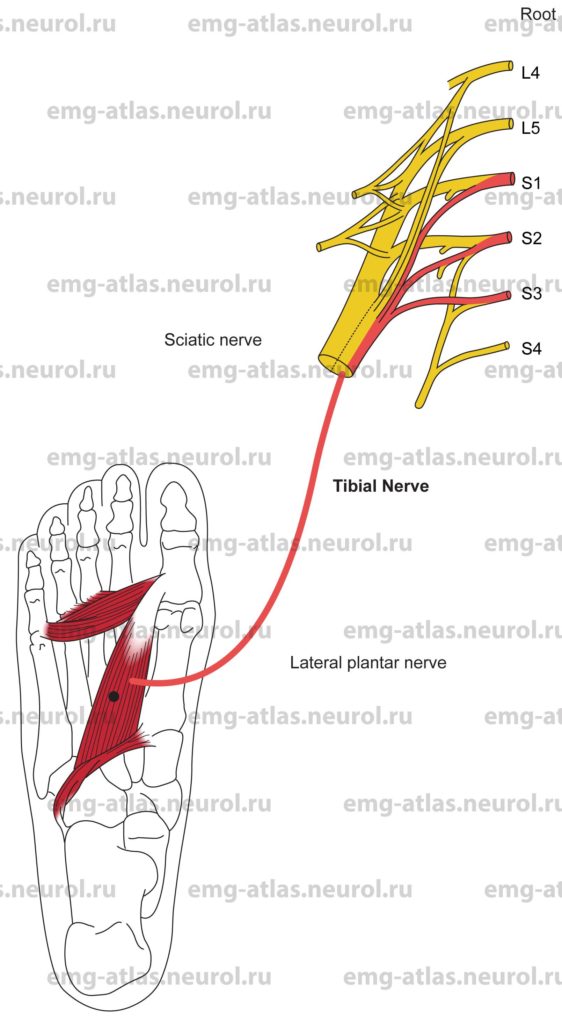
Diagram of the tibial nerve (posterior view) and its branches.
The tibial nerve (also known as the posterior tibial nerve) is the larger sciatic division and is formed by the fourth and fifth lumbar and the first to third sacral ventral rami (Gray’s Anatomy, 1995). It descends along the back of the thigh and the popliteal fossa to the distal border of the popliteus muscle, passing anterior to the aponeurotic arch of the soleus with the popliteal artery and vein to enter the leg. In the distal thigh, it is overlapped by the hamstring muscles, but becomes more superficial in the popliteal fossa, where it is lateral to the popliteal vessels, becoming superficial to them at the knee and crossing to the medial side of the vessels as it enters the leg. In the distal fossa, it is overlapped by the junction of the two heads of the gastrocnemius muscles.
In the leg, the tibial nerve descends with the posterior tibial artery and vein, crossing lateral to the vessels. Proximally, the nerve is deep to the soleus and gastrocnemius, but in the distal one-third of the leg it is covered only by skin and fascia, sometimes overlapped by the flexor hallucis longus. It reaches the medial malleolus, ending under the flexor retinaculum, where it divides into medial and lateral plantar nerves.
The tibial nerve gives off articular branches to the knee joint. Just before it divides it also supplies the ankle joint. Most of the articular branches are nociceptive in nature. Muscular branches supply the two heads of the gastrocnemius, plantaris (a small, almost vestigial muscle that is the lower limb equivalent of the palmaris longus), soleus, popliteus, tibialis posterior, flexor digitorum longus, and flexor hallucis longus. Cutaneous branches include the sural and medial calcaneal nerves. The sura nerve is joined by a sural communicating branch of the common peroneal nerve and descends along the calf and lateral border of the Achilles tendon to the region between the lateral malleolus and the calcaneous. It supplies the posterior and lateral skin of the distal third of the leg, the skin overlying the lateral malleolus, and the lateral aspect of the foot and little toe (Sunderland, 1968). The medial calcaneal branch supplies the skin of the heel and the medial side of the sole.
The medial plantar nerve also gives off articular, cutaneous, and muscular branches. The cutaneous branches supply the skin of the sole of the foot, including the digital branches to the hallux, the second, third, and half of the fourth toe (the digital branches of the medial plantar nerve are like those of the median nerve). Muscular branches supply the abductor hallucis, flexor digitorum brevis, flexor hallucis brevis, and the first lumbrical (the muscular branches of the medial plantar nerve also correspond closely with those of the median nerve).
The lateral plantar nerve supplies the skin of the fifth toe, the lateral half of the fourth toe, and the lateral part of the sole of the foot (like the ulnar nerve in the hand). Muscular branches supply most deep muscles of the foot, including the flexor digitorum accessorius, abductor digiti minimi (quinti), flexor digiti minimi brevis, interossei, second to fourth lumbricals, and adductor hallucis.
The tibial nerve, or its branches, may be involved by penetrating injuries at any level. Of the two terminal divisions of the sciatic nerve, however, the tibial is the more deeply situated and better protected (Sunderland, 1968). At the ankle, the tibial nerve may rarely be subjected to compression beneath the flexor retinaculum (tarsal tunnel). This may result in the tarsal tunnel syndrome.
Tarsal Tunnel Syndrome
Etiology
Tarsal tunnel syndrome is caused by compression of the tibial nerve or its branches in the tarsal tunnel.
General Comments
Tarsal tunnel syndrome is a rare entrapment neuropathy.
Symptoms usually involve one foot (Dawson et al., 1990).
Predisposing conditions include trauma, such as fracture or dislocation at the ankle, deformity or hypermobility at the ankle, peripheral neuropathy, rheumatoid arthritis, and hyperlipidemia.
Radiologic studies of the ankle may reveal evidence of degenerative arthritis, old fractures, bone spicules, or accessory ossicals (DeLisa and Saeed, 1983).
Clinical Features
Pain, reportedly burning in quality, occurs in the sole of the foot.
Patients may awaken at night with symptoms (nocturnal paresthesias).
Numbness may involve the medial plantar or lateral plantar areas and occasionally the whole surface of the foot, including the medial calcaneal distribution (Dawson et al., 1990).
Tinel’s sign over the tarsal tunnel may be present (Oh et al., 1979).
Weakness and atrophy of the intrinsic foot muscles are difficult to detect clinically.
Electrodiagnostic Strategy
Use nerve conduction studies to confirm a focal lesion of the tibial sensory or motor fibers in the tarsal tunnel. Techniques have been developed for identifying conduction abnormalities within the tarsal tunnel (Oh et al., 1979; DeLisa and Saeed, 1983).
Perform EMG needle examination in the foot muscles innervated by both the medial and lateral plantar nerves. In tarsal tunnel syndrome associated with loss of motor fibers, EMG may show neurogenic changes (i.e., spontaneous activity, abnormal motor unit potentials, and abnormal recruitment).
If EMG examination of the foot muscles is abnormal, study the proximal tibial–innervated muscles to exclude a tibial nerve lesion above the ankle. Compare with the findings in the other foot because tarsal tunnel syndrome is often unilateral. Also, study the S1 and S2 muscles innervated by other nerves to exclude radiculopathy.
Anatomical Illustrations
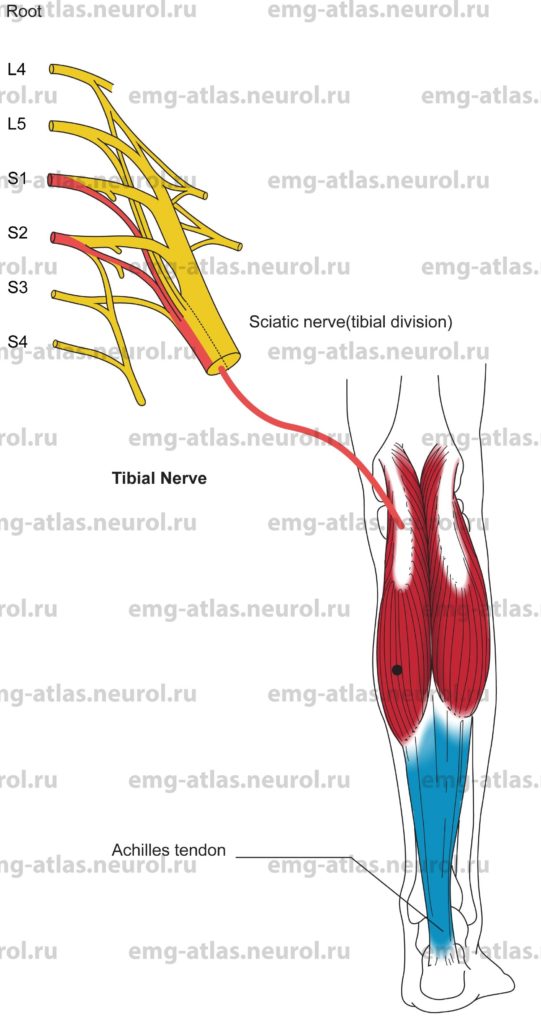
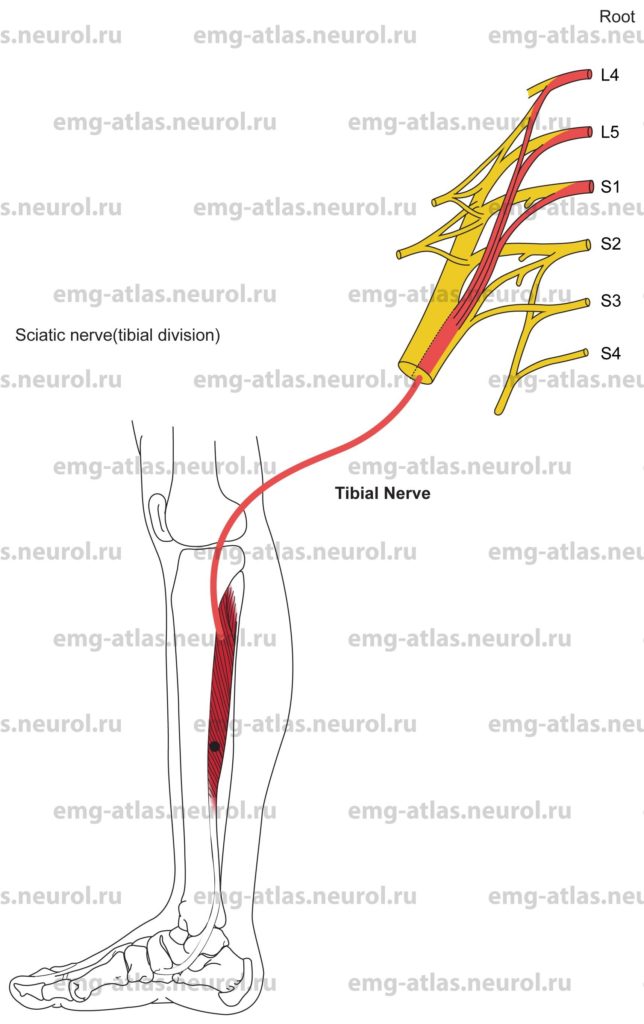
Gastrocnemius, Medial Head
Innervation
Innervation is via the tibial nerve, tibial division of the sciatic nerve, sacral plexus, and roots S1, S2.
Origin
The medial head of the gastrocnemius originates at the medial condyle of the femur.
Insertion
Insertion is at the calcaneus via the Achilles tendon.
Activation Maneuver
Plantar flexion of the foot against resistance activates the muscle.
EMG Needle Insertion
Insert the needle into the medial mass of the calf.
Pitfalls
If the needle is inserted too deeply, it may be in the soleus, which is also supplied by the tibial nerve and S1, S2.
If the needle is inserted still deeper, it may be in the flexor digitorum longus or tibialis posterior (both muscles supplied by the tibial nerve and L5, S1). These muscles may show neurogenic changes on needle examination in an L5 radiculopathy.
Clinical Comments
Neurogenic changes in the medial gastrocnemius on needle examination may be seen with lesions of the tibial nerve, sciatic nerve, sacral plexus, and S1 or S2 roots.
Anatomical Illustrations
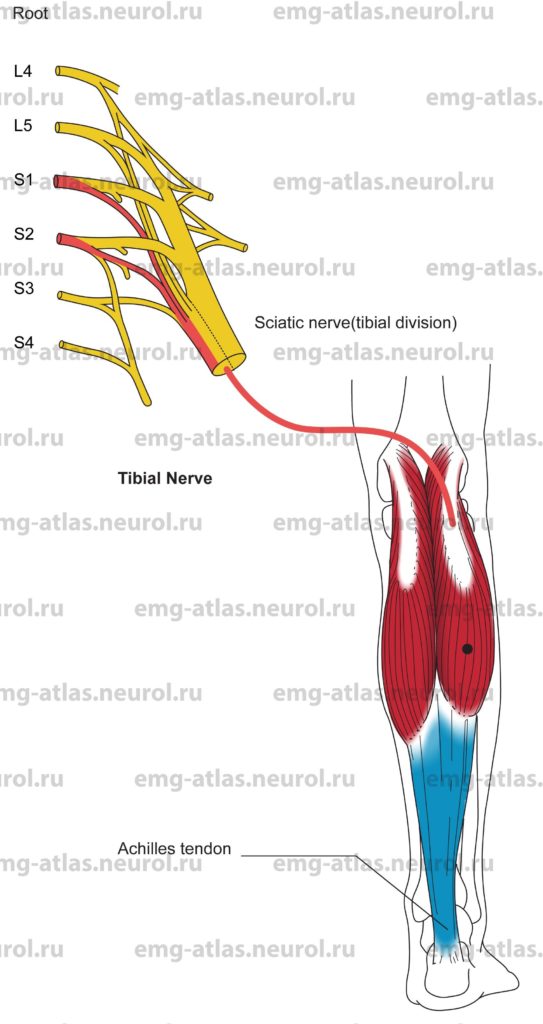
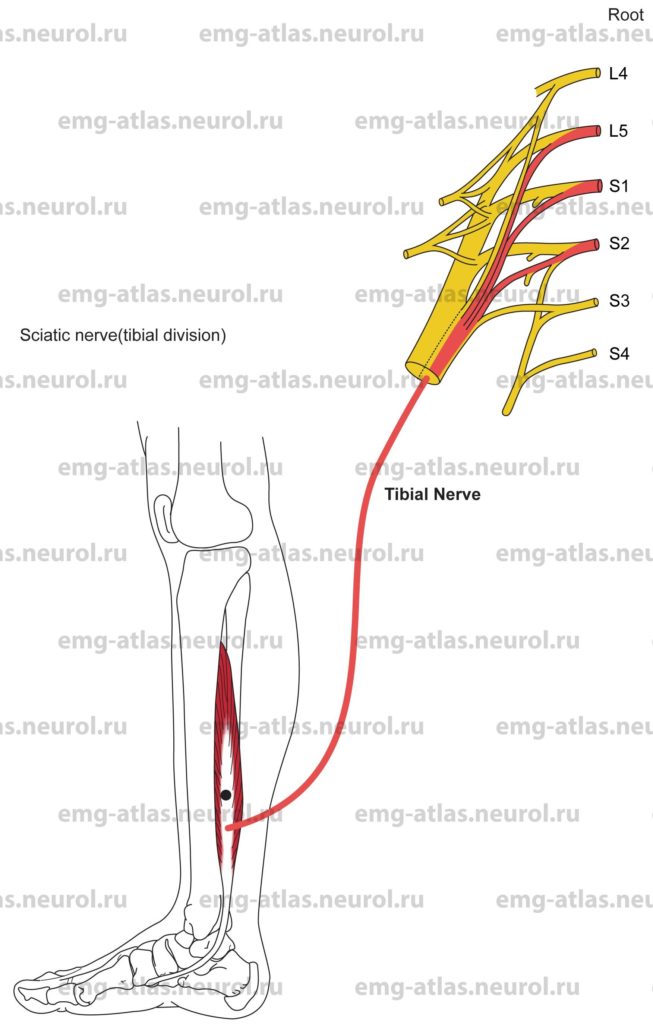
Gastrocnemius, Lateral Head
Innervation
Innervation is via the tibial nerve, tibial division of the sciatic nerve, sacral plexus, and roots S1, S2.
Origin
The lateral head of the gastrocnemius originates at the lateral condyle of the femur.
Insertion
Insertion is at the calcaneus via the Achilles tendon.
Activation Maneuver
Plantar flexion of the foot against resistance activates the muscle.
EMG Needle Insertion
Insert the needle into the lateral mass of the calf.
Pitfalls
If the needle is inserted too deeply, it may be in the soleus, which is also supplied by the tibial nerve and S1, S2.
If the needle is inserted too laterally and anteriorly, it may be in the peroneus longus or brevis, which are supplied by the superficial peroneal nerve. The outer border of the lateral gastrocnemius contacts the peronei muscles.
Clinical Comments
Neurogenic changes in this muscle on needle examination may be seen with lesions of the tibial nerve, sciatic nerve, sacral plexus, and S1 or S2 roots.
Anatomical Illustrations
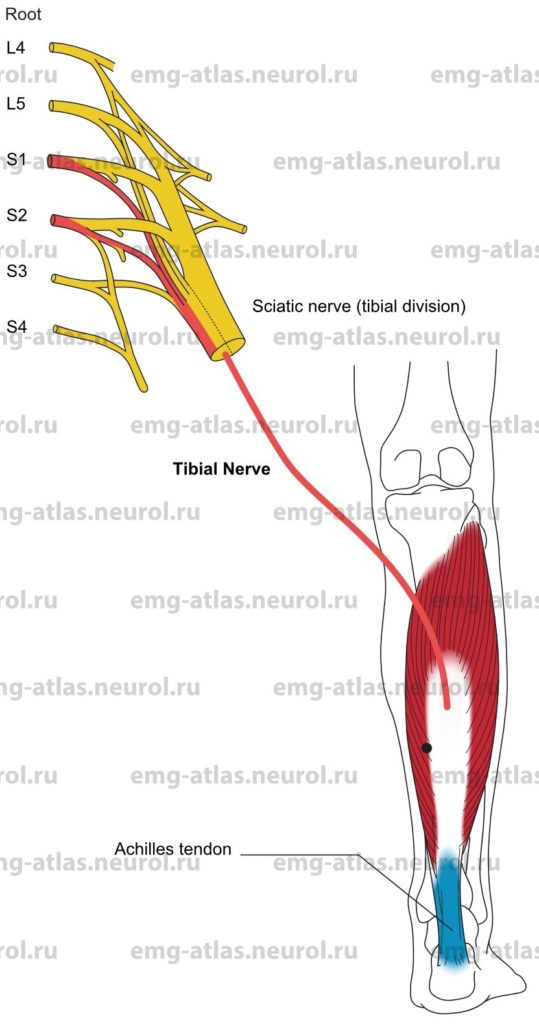
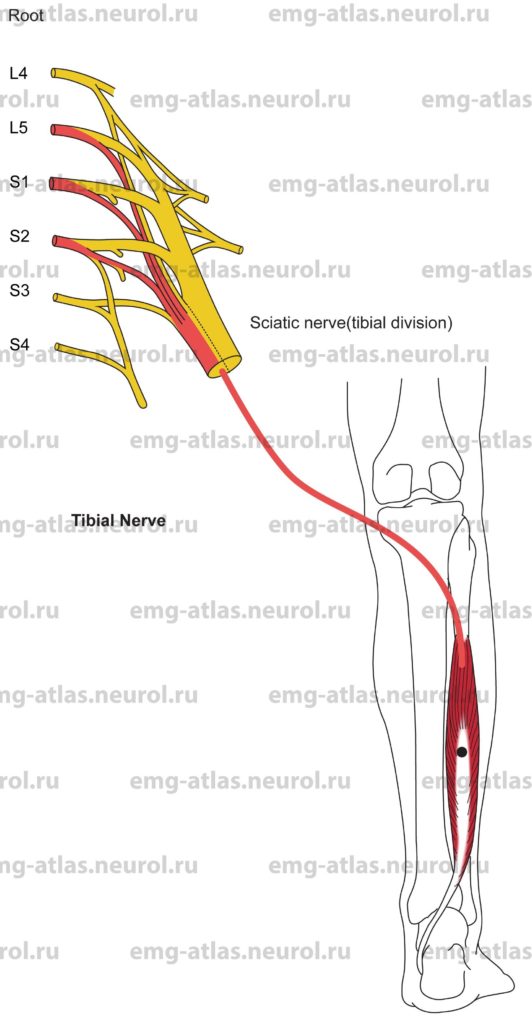
Soleus
Innervation
Innervation is via the tibial nerve, tibial division of the sciatic nerve, sacral plexus, and roots S1, S2 (may also receive an L5 contribution from the internal popliteal branch).
Origin
The soleus originates at the head of the fibula and the upper third of the posterior surface of its shaft and from the oblique line of the tibia and middle third of the medial surface of its shaft.
Insertion
Insertion is at the calcaneus via the Achilles tendon. Note: The Achilles tendon is the common tendon of the medial and lateral gastrocnemius and soleus muscles. These three muscles are sometimes referred to as the triceps surae.
Activation Maneuver
Plantar flexion of the foot against resistance activates the muscle.
EMG Needle Insertion
Insert the needle just distal to the belly of the medial gastrocnemius, medial to the Achilles tendon.
Pitfalls
If the needle is inserted too deeply, it may be in the flexor digitorum longus or tibialis posterior, which are supplied by the tibial nerve and L5, S1. These muscles may show neurogenic changes on needle examination in an L5 radiculopathy.
Clinical Comments
Neurogenic changes in the soleus on needle examination may be seen with lesions of the tibial nerve, sciatic nerve, sacral plexus, and S1 or S2 roots. The soleus usually does not show neurogenic changes in an L5 radiculopathy.
Anatomical Illustrations
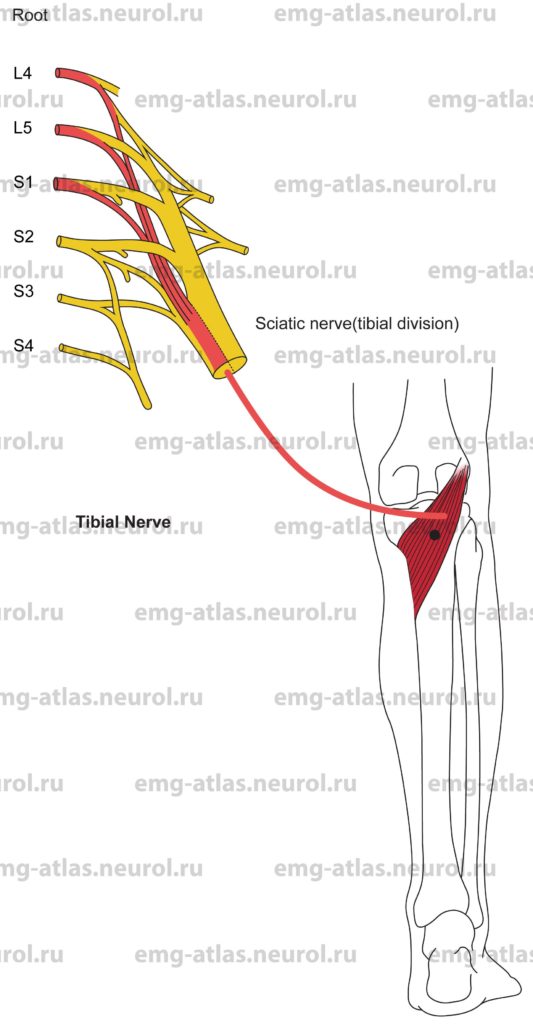
Tibialis Posterior
Innervation
Innervation is via the tibial nerve, tibial division of the sciatic nerve, sacral plexus, and roots L5, S1 (may also receive L4 contribution).
Origin
The tibialis posterior originates at the posterior surface of the interosseous membrane throughout the entire length except at the lowest part, the posterior surface of the shaft of the tibia (between the oblique line and the junction of the middle and lower thirds of the shaft), and the upper two-thirds of the medial surface of the fibula.
Insertion
Insertion is at the tuberosity of the navicular and medial cuneiform bones (the tendon also gives off fibrous expansions to the sustentaculum tali of the calcaneus, middle and lateral cuneiform and cuboid bones, and bases of the second through fourth metatarsal bones).
Activation Maneuver
Inversion of the foot activates the muscle.
EMG Needle Insertion
Insert the needle 1-2 cm medial to the margin of the tibia at the junction of the upper two-thirds with the lower third of the shaft. Direct the needle obliquely underneath the shaft) through the soleus and flexor digitorum muscles.
Pitfalls
If the needle is inserted too superficially, it will be in the flexor digitorum longus also supplied by the tibial nerve and L5, S1) or soleus (supplied by the tibial nerve and S1, S2).
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the tibial nerve, sciatic nerve, sacral plexus, and L5, S1 roots.
The tibialis posterior and flexor digitorum longus are usually abnormal in severe “foot drop” due to L5 radiculopathy. Conversely, these muscles are normal in foot drop due to peroneal mononeuropathy.
Anatomical Illustrations
Flexor Digitorum Longus
Innervation
Innervation is via the tibial nerve, tibial division of the sciatic nerve, sacral plexus, and roots L5, S1 (may also receive S2 contribution).
Origin
The flexor digitorum longus originates at the posterior surface of the midshaft of the tibia immediately below the oblique line.
Insertion
Insertion is at the bases of the distal phalanges of the four lesser toes.
Activation Maneuver
Flexion of the four lesser toes without plantar flexion or inversion the foot (i.e., do not coactivate the soleus or tibialis posterior muscles) activates the muscle.
EMG Needle Insertion
Insert the needle 1-2 cm medial to the margin of the tibia at the junction of the upper two-thirds with the lower third of the shaft. Direct the needle obliquely underneath the shaft) through the soleus muscle.
Pitfalls
If the needle is inserted too superficially, it will be in the soleus muscle (supplied by the tibial nerve and S1, S2).
If the needle is inserted too deeply, it will be in the tibialis posterior (also supplied by the tibial nerve and L5, S1).
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the tibial nerve, sciatic nerve, sacral plexus, and L5, S1 roots.
The tibialis posterior and flexor digitorum longus are usually abnormal in severe «foot drop» due to L5 radiculopathy. Conversely, these muscles are normal in foot drop due to peroneal mononeuropathy.
Anatomical Illustrations
Flexor Hallucis Longus
Innervation
Innervation is via the tibial nerve, tibial division of the sciatic nerve, sacral plexus, and roots L5, S1, S2.
Origin
The flexor hallucis longus originates at the posterior surface of the distal two-thirds of the shaft of the fibula and the interosseous membrane.
Insertion
Insertion is at the base of the distal phalanx of the great toe.
Activation Maneuver
Flexion of the great toe without coactivation of other muscles activates the flexor hallucis longus.
EMG Needle Insertion
Insert the needle into the posterolateral aspect of the leg, at the junction of the upper two-thirds with the lower third. The muscle belly is situated deep on the fibular side of the leg and is larger than the flexor digitorum or tibialis posterior.
Pitfalls
If the needle is inserted too superficially, it will be in the soleus muscle (supplied by the tibial nerve and S1, S2).
If the needle is inserted too medially and deeply, it will be in the tibialis posterior also supplied by the tibial nerve and L5, S1).
If the needle is inserted too laterally, it will be in the peroneus longus or brevis (supplied by the superficial peroneal nerve and L5, S1, S2). The outer border of the flexor hallucis longus abuts the peronei muscles.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the tibial nerve, sciatic nerve, sacral plexus, and L5, S1, or S2 roots.
Anatomical Illustrations
Popliteus
Innervation
Innervation is via the tibial nerve, tibial division of the sciatic nerve, the sacral plexus, and roots L4, L5, S1.
Origin
The popliteus originates at the lateral condyle of the femur and the posterior ligament of the knee joint.
Insertion
Insertion is at the posterior surface of the shaft of the tibia above the oblique line.
Activation Maneuver
Flexion of the knee joint activates the muscle. The popliteus produces a slight inward rotation of the tibia, which is essential during the early stages of bending the knee.)
EMG Needle Insertion
Insert the needle into the floor of the popliteal fossa in the proximal leg midway between the insertions of the outer and inner hamstring tendons.
Pitfalls
Testing of the popliteus is rarely useful in routine electromyography due to the muscle’s thinness and proximity to the popliteal vessels.
If the needle is inserted too superficially, it will be in the gastrocnemius muscles supplied by the tibial nerve and S1, S2).
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the tibial nerve, sciatic nerve, sacral plexus, and roots L4, L5, or S1.
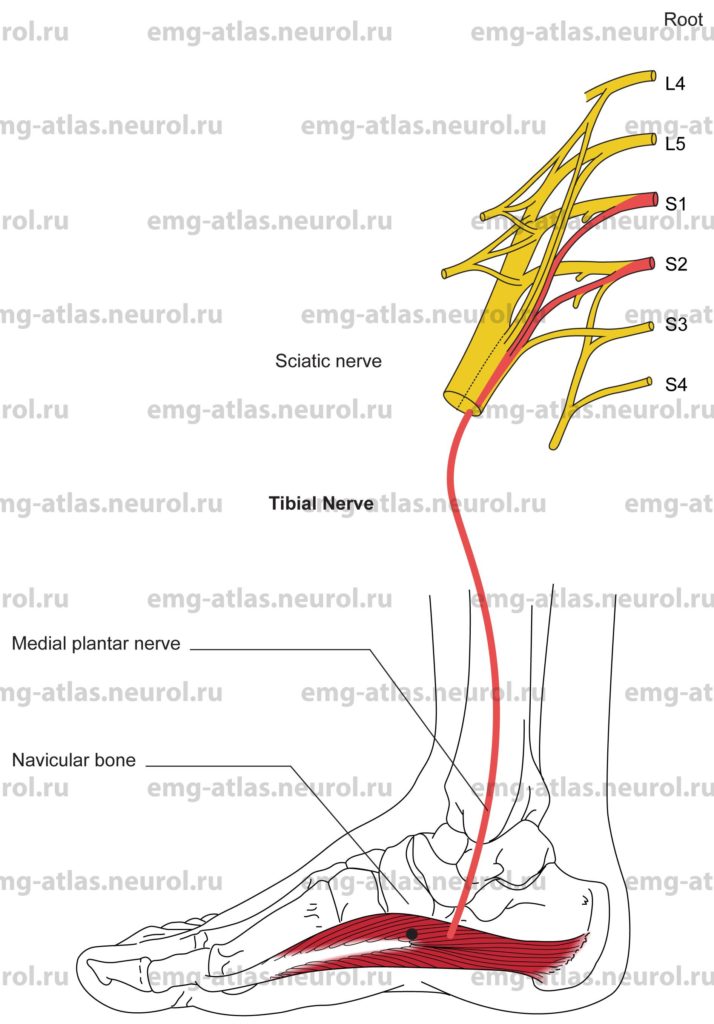
Anatomical Illustrations
Abductor Hallucis
Innervation
Innervation is via the medial planter nerve, tibial nerve, tibial division of the sciatic nerve, sacral plexus, and roots S1, S2.
Origin
The abductor hallucis originates at the medial process of the calcaneus (heel bone).
Insertion
Insertion is at the base of the first phalanx of the great toe.
Activation Maneuver
Abduction of the great toe activates the muscle.
EMG Needle Insertion
Insert the needle into the muscle belly directly beneath the navicular bone.
Pitfalls
Some subjects may not be able to voluntarily activate this muscle.
If the needle is inserted too deeply, it may be in the flexor hallucis brevis muscle also supplied by the medial plantar nerve and S1, S2).
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the medial plantar nerve, tibial nerve, sciatic nerve, sacral plexus, and S1 or S2 root.
The abductor hallucis is involved in the tarsal tunnel syndrome.
The abductor hallucis is also involved early in length-dependent peripheral neuropathies.
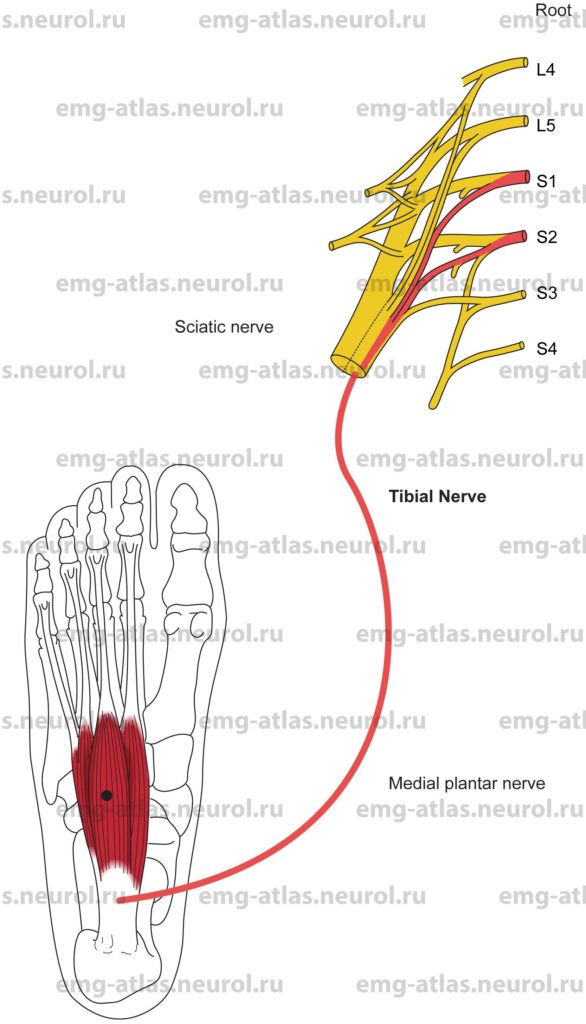
Anatomical Illustrations
Flexor Digitorum Brevis
Innervation
Innervation is via the medial plantar nerve, tibial nerve, tibial division of the sciatic nerve, sacral plexus, and roots S1, S2.
Origin
The flexor digitorum brevis originates at the medial process of the calcaneus (heel bone) and the central part of the plantar aponeurosis.
Insertion
Insertion is at the bases of the middle phalanges of the second, third, fourth, and fifth toes.
Activation Maneuver
Flexion of the four lesser toes activates the muscle.
EMG Needle Insertion
Insert the needle midway between the third metatarsal head and the calcaneus. The muscle is superficial.
Pitfalls
If the needle is inserted too laterally, it may be in the abductor digiti minimi (quinti) or other muscles innervated by the lateral plantar nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the medial plantar nerve, tibial nerve, sciatic nerve, sacral plexus, and S1 or S2 root.
The flexor digitorum brevis is involved in tarsal tunnel syndrome.
The flexor digitorum brevis is also involved early in length-dependent peripheral neuropathies.
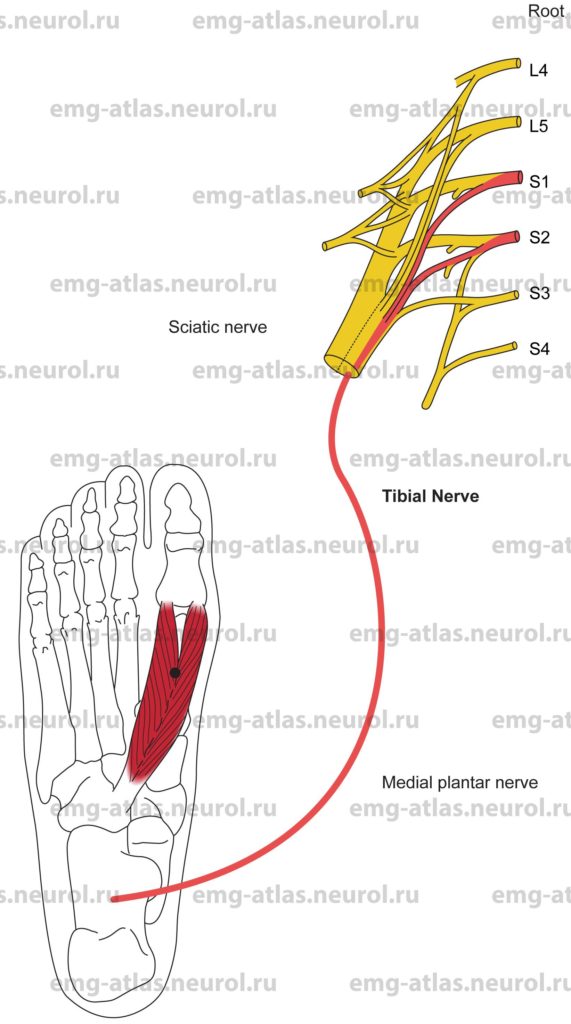
Anatomical Illustrations
Flexor Hallucis Brevis
Innervation
Innervation is via the medial plantar nerve, tibial nerve, tibial division of the sciatic nerve, sacral plexus, and roots S1, S2.
Origin
The flexor hallucis brevis originates at the plantar surface of the cuboid, the lateral cuneiform, and the tendon of the tibialis posterior.
Insertion
Twin tendons attach to the base of the first phalanx of the great toe.
Activation Maneuver
Flexion of the great toe at the metatarsophalangeal joint activates the muscle.
EMG Needle Insertion
Insert the needle into the plantar surface of the foot 2 cm proximal to the first metatarsal head.
Pitfalls
If the needle is inserted too laterally, it may be in the adductor hallucis (supplied by the lateral plantar nerve and S1, S2, S3).
The abductor hallucis is superficial to the flexor hallucis brevis, but it is also innervated by the medial plantar nerve and S1, S2.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the medial plantar nerve, tibial nerve, sciatic nerve, sacral plexus, and S1 or S2 root.
The flexor hallucis brevis is involved in the tarsal tunnel syndrome.
The flexor hallucis brevis is also involved early in length-dependent peripheral neuropathies.
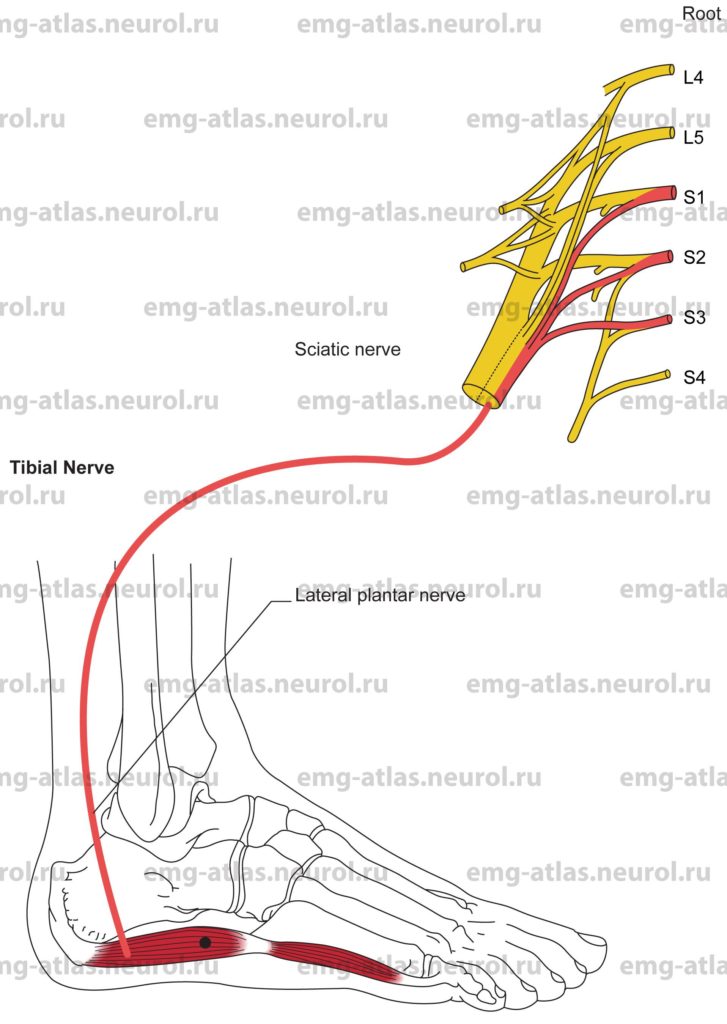
Anatomical Illustrations
Abductor Digiti Minimi (Quinti)
Innervation
Innervation is via the lateral plantar nerve, tibial nerve, tibial division of the sciatic nerve, sacral plexus, and roots S1, S2, S3.
Origin
The abductor digiti minimi (quinti) originates at the medial and lateral processes of the calcaneus (heel bone) and the plantar aponeurosis. This muscle lies superficially along the lateral border of the foot.
Insertion
Insertion is at the lateral side of the base of the proximal phalanx of the fifth toe.
Activation Maneuver
Abduction or flexion of the fifth toe activates the muscle.
EMG Needle Insertion
Insert the needle along the lateral border of the foot midway between the fifth metatarsal head and the calcaneus.
Pitfalls
There are no pitfalls. If the needle is inserted too deeply, it will still be in muscles innervated by the lateral plantar nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the lateral plantar nerve, tibial nerve, sciatic nerve, sacral plexus, and roots S1, S2, or S3.
The abductor digiti minimi (quinti) is involved in the tarsal tunnel syndrome.
The abductor digiti minimi (quinti) is also involved early in length-dependent peripheral neuropathies.
Anatomical Illustrations
Adductor Hallucis
Innervation
Innervation is via the lateral plantar nerve, tibial nerve, tibial division of the sciatic nerve, sacral plexus, and roots S1, S2, S3.
Origin
The oblique head originates from the bases of the second, third, and fourth metatarsal bones and from the fibrous sheath of the tendon of the peroneus longus.
The transverse head originates from the plantar metatarsophalangeal ligaments of the third, fourth, and fifth toes.
Insertion
Insertion is at the medial side of the base of the proximal phalanx of the great toe and the lateral sesamoid bone of the great toe.
Activation Maneuver
Adduction of the great toe activates the muscle.
EMG Needle Insertion
Insert the needle 4-5 cm proximal to the second metatarsal head to a depth of 2 cm or more (the muscle lies deep). This will access the thick, fleshy oblique head.
Pitfalls
If the needle is inserted too medially, it may be in the flexor hallucis brevis, which is innervated by the medial planter nerve.
If the needle is inserted too superficially, it may be in the first lumbrical, which is innervated by the medial plantar nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the lateral plantar nerve, tibial nerve, sciatic nerve, sacral plexus, and roots S1, S2, or S3.
The adductor hallucis is involved in the tarsal tunnel syndrome.
The adductor hallucis is also involved early in length-dependent peripheral neuropathies.