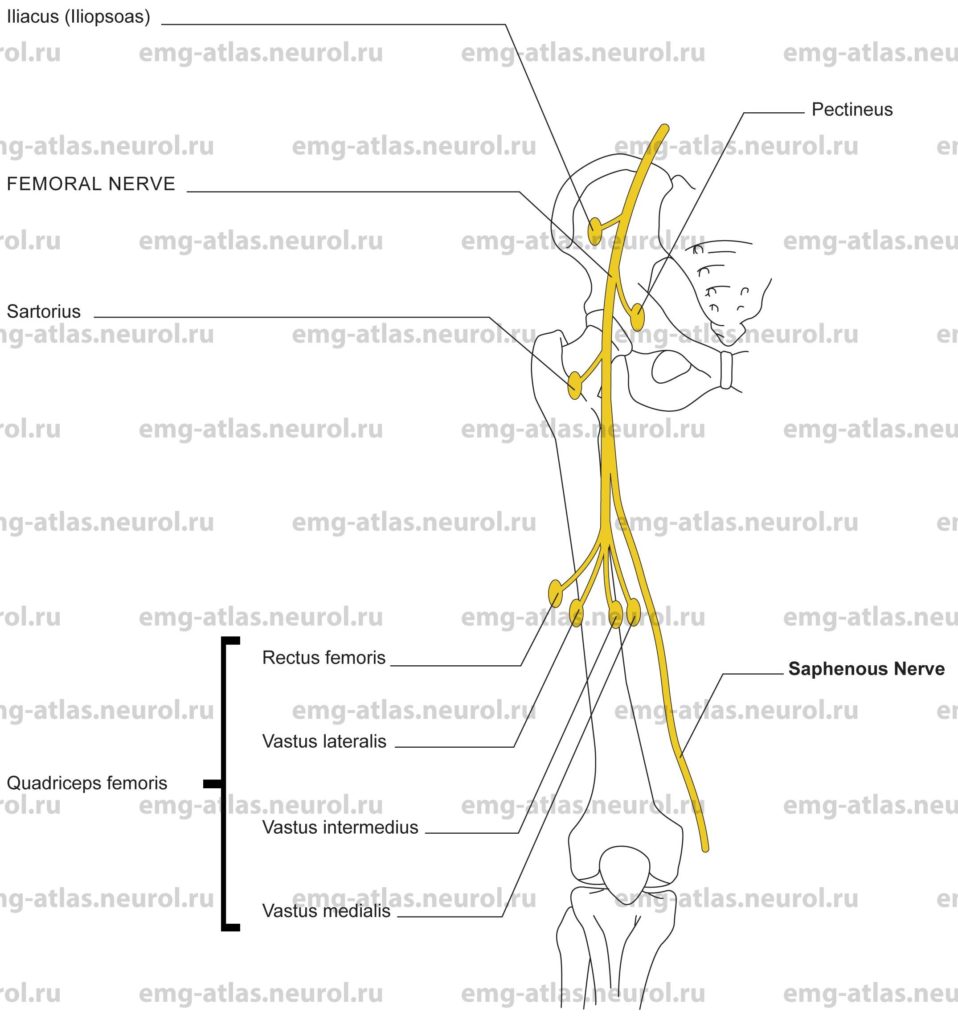
Diagram of the femoral nerve (anterior view) and the muscles that it supplies.
The femoral nerve is the largest branch of the lumbar plexus. It arises from the posterior division of the second to fourth ventral rami, within the substance of the psoas major. It emerges from the psoas at its lower outer border in a groove between this muscle and the iliacus and descends along the groove to pass beneath the inguinal ligament to enter the thigh. In the iliac fossa, it supplies small branches to the iliacus muscle (the iliacus and psoas major act together, the combination being referred to as the iliopsoas muscle; Gray’s Anatomy, 1995). While beneath the inguinal ligament, it gives off a branch that courses medially behind the femoral sheath to supply the pectineus muscle.
Note: The short muscles around the hip joint—pectineus, obturator externus, quadratus femoris, gemellus superior, gemellus inferior, obturator internus, and piriformis—are largely innaccessible to direct observation. Because of the potential complications presented by their intimate relationship to important neurovascular structures, there is a total lack of EMG data for humans (Gray’s Anatomy, 1995).
On entering the femoral triangle, the femoral nerve lies on the iliacus muscle lateral to the femoral artery. About 4 cm distal to the inguinal ligament, it divides into anterior and posterior divisions that, in turn, subdivide to give further branches. The anterior division divides almost immediately into a muscular branch to the sartorius and two cutaneous branches, the intermediate and medial cutaneous nerves of the thigh.
The intermediate cutaneous nerve of the thigh provides sensation to the anterior surface of the thigh as far distally as the knee. The medial cutaneous nerve of the thigh innervates the medial and anteromedial aspects of the thigh and continues on to innervate the medial aspect of the leg just below the knee. The posterior division immediately divides into the saphenous branch and muscular branches. The saphenous nerve descends to the knee where it becomes subcutaneous. It joins the saphenous vein, which it accompanies down the medial aspect of the leg. Branches of the saphenous nerve provide sensation to the skin on the medial aspect of the leg, and continue on to innervate the skin over the medial ankle and a portion of the medial foot. Muscular branches arise in spray fashion from the parent division and innervate the rectus femoris, vastus lateralis, vastus intermedius, and vastus medialis.
Anatomical features of clinical importance relate to the posterior abdominal wall, where a retroperitoneal hematoma or hemorrhage may compress the nerve (Sunderland, 1968). The appearance of signs or symptoms of a femoral nerve lesion in a patient with hemophilia or who is receiving anticoagulant therapy strongly suggests involvement of the nerve by a hematoma or hemorrhage. Compression of the nerve may also occur in this region from a benign or malignant tumor or an abscess. Beneath the inguinal ligament, the nerve may rarely be injured during inguinal or femoral hernia repair. Postsurgical femoral mononeuropathy has also been reported following positioning on the operating table in which the thigh is acutely flexed as in the lithotomy position. In these cases, nerve involvement is likely related to acute angulation across the inguinal ligament (Sunderland, 1968). In the femoral triangle, gunshot wounds and other penetrating injuries are often fatal because the femoral artery and vein are also severed. Injuries distal to the site where muscular branches arise in spray fashion result in variable involvement of the branches; some will be spared while others will be involved depending on the precise site and nature of the injury.
Femoral nerve lesion
Etiology
Retroperitoneal hematomas or hemorrhages that cause a femoral nerve lesion are usually seen in patients with hemophilia or who are receiving anticoagulant therapy.
Retroperitoneal tumors (benign or malignant) and abscessess are causative.
Femoral nerve lesions can be caused iatrogenically (e.g., (herniorraphy, appendectomy, hysterectomy, femoral angiography, postanesthesia compression due to acute angulation across the inguinal ligament).
Other causes of femoral nerve lesions include (1) penetrating injuries, (2) aneurysm of the femoral artery, (3) neuralgic amyotrophy, and (4) diabetic amyotrophy (femoral nerve involvement is common).
General Comments
In diabetic amyotrophy, muscle weakness may first appear in the quadriceps muscles. Diabetic amyotrophy, however, is not simply a femoral mononeuropathy. Additional proximal muscles are involved, including gluteal, hamstring, adductor, and iliopsoas muscles (Chokroverty and Sander, 1996).
Clinical Features
The quadriceps muscles atrophy.
Paresis or paralysis of the quadriceps muscles produces weakness or an inability to extend the leg.
Paresis or paralysis of the iliopsoas, rectus femoris, and sartorius produces weakness during thigh flexion. If the iliopsoas is spared, as in a more distal lesion, loss of rectus femoris and sartorius is without noticeable effect (Sunderland, 1968).
Numbness or a loss of sensation can occur in the anterior and medial aspects of the thigh and in the medial aspect of the leg.
There is loss of the patellar tendon reflex.
Electrodiagnostic Strategy
Use nerve conduction studies (saphenous sensory response and femoral motor response) to help determine a lesion of the femoral nerve or its branches.
Perform EMG needle examination in thigh muscles innervated by the femoral nerve or its branches. In lesions associated with loss of motor fibers, EMG may show neurogenic changes (i.e., fibrillation potentials, polyphasic motor unit potentials, and neurogenic recruitment).
If EMG of the quadriceps muscles is abnormal, study other proximal muscles (gluteal, hamstring, and adductors) and paraspinal muscles to exclude plexus or root involvement.
Anatomical Illustrations
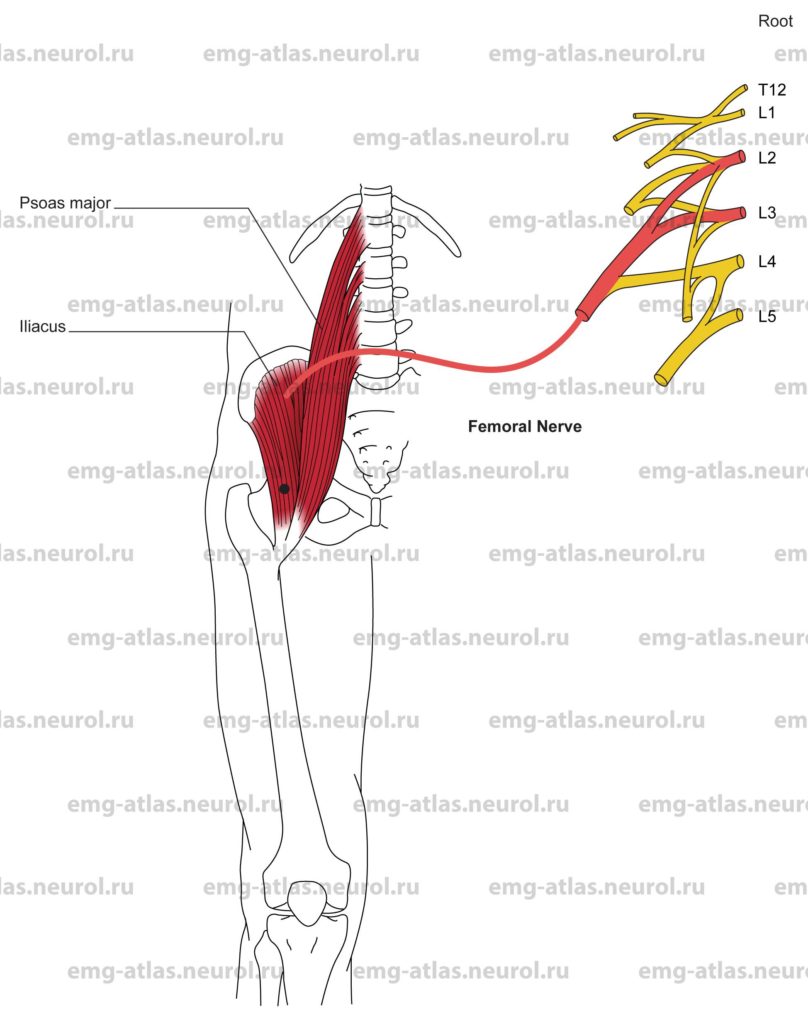
Iliacus (Iliopsoas)
Innervation
Innervation is via the femoral nerve, posterior division of the lumbar plexus, and roots L2, L3.Note: Iliacus and psoas major act together, the combination being referred to as Hiopsoas. However, direct branches from ventral rami of the lumbar spinal nerves L1, L2and L3supply the psoas major.
Origin
The iliacus originates at the superior two-thirds of the iliac fossa, inner lip of the iliac crest, and upper surface of the lateral sacrum.
The psoas major originates at the Transverse processes and bodies of all lumbar vertebrae and the body of the twelfth thoracic vertebra.
Insertion
The iliacus and psoas major insert together into the lesser trochanter of the femur (iliacus fibers are lateral; psoas fibers are medial).
Activation Maneuver
Flexion of the thigh upon the pelvis activates the muscle.
EMG Needle Insertion
Insert the needle 3-4 cm lateral to the femoral artery pulse just below the inguinal ligament.
Pitfalls
If the needle is inserted too medially, it may penetrate the femoral nerve or artery.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the femoral nerve within the abdomen (retroperitoneal hematoma or mass lesion), posterior division of lumbar plexus, or L2, L3 roots.
Anatomical Illustrations
Pectineus
Innervation
Innervation is via the femoral nerve, posterior division of the lumbar plexus, and roots L2, L3. This muscle may also receive a branch from the obturator nerve (Gray’s Anatomy, 1995).
Origin
The pectineus originates from the pecten pubis (superior ramus of the pubis).
Insertion
Insertion is along a line from the lesser trochanter to the linea aspera of the femur.
Activation Maneuver
Adduction and flexion of the thigh activate the muscle.
EMG Needle Insertion
Insert the needle 2-3 cm medial to the femoral artery pulse just below the inguinal ligament.
Pitfalls
If the needle is inserted too laterally, it may penetrate the femoral vein or artery; this muscle is often avoided in the EMG assessment due to its relationship with the neurovascular bundle, which traverses the lateral aspect of the muscle (Gray’s Anatomy, 1995).
If the needle is inserted too medially, it may be in the adductor longus, which is supplied by the obturator nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the femoral nerve within the abdomen (retroperitoneal hematoma or mass lesion), posterior division of the lumbar plexus, or L2, L3 roots.
Anatomical Illustrations
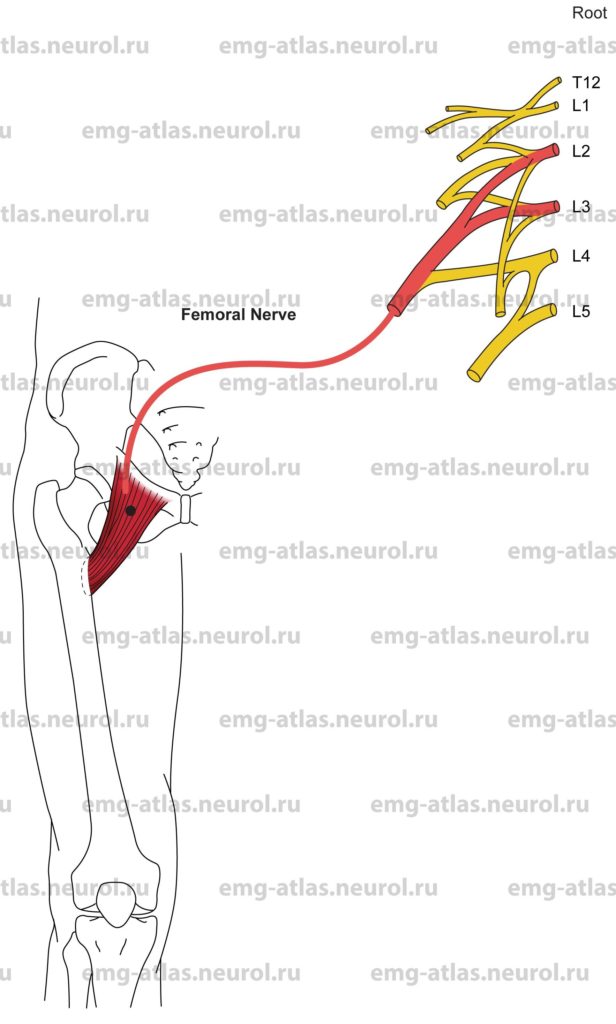
Sartorius
Innervation
Innervation is via the femoral nerve, posterior division of the lumbar plexus, and roots L2, L3.
Origin
The sartorius originates at the anterior superior iliac spine.
Insertion
Insertion is at the proximal medial surface of the tibia.
Activation Maneuver
Flexion of the thigh and flexion of the knee activate the muscle. (The sartorius is a narrow strap muscle that crosses the hip and knee joints; it is the longest muscle of the body.)
EMG Needle Insertion
Insert the needle 6-7 cm distal to the anterior superior iliac spine along a line to the medial epicondyle of the tibia.
Pitfalls
If the needle is inserted too laterally, it may be in the tensor fasciae latae, which is innervated by the superior gluteal nerve.
If the needle is inserted too medially or deeply, it may be in the iliopsoas or rectus femoris, respectively, which are also supplied by the femoral nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the femoral nerve, posterior division of the lumbar plexus, or L2, L3 roots.
Anatomical Illustrations
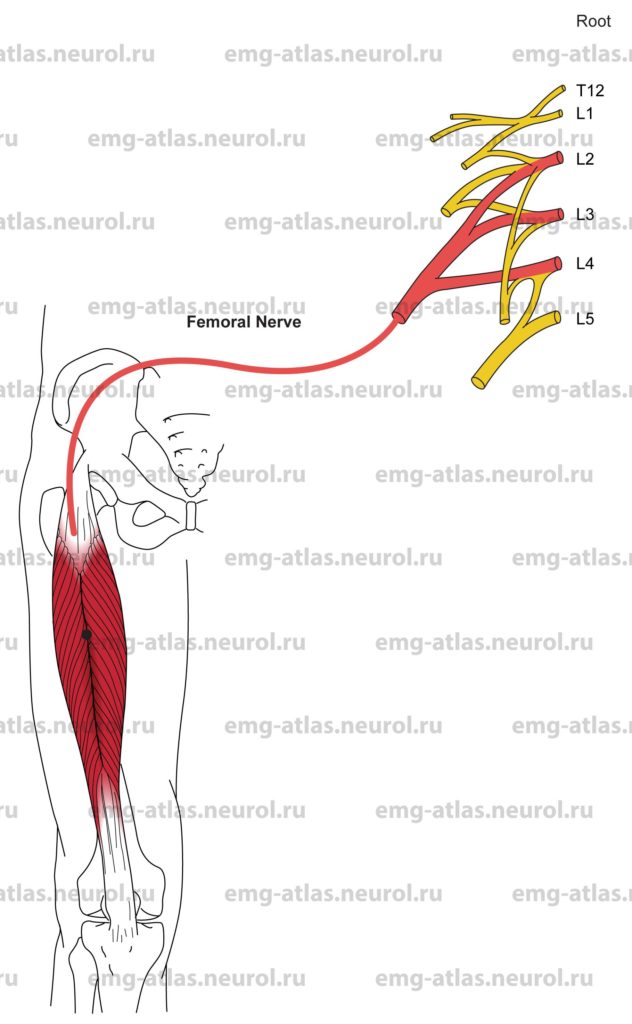
Rectus Femoris
Innervation
Innervation is via the femoral nerve, posterior division of the lumbar plexus, and roots L2, L3, L4.
Origin
The rectus femoris originates at the anterior inferior iliac spine and a groove above the acetabulum of the ilium. This is the only quadriceps muscle that arises from the ilium; the other three arise from the shaft of the femur. The muscle travels straight down the middle of the thigh, hence its name rectus femoris.
Insertion
Insertion is at the base of the patella via the quadriceps tendon. Note: The tendons of the four quadriceps unite to form a single strong tendon attached to the base of the patella. The patella is in fact a sesamoid bone in the quadriceps tendon, and the ligamentum patellae, which extends to insert on the tubercle of the tibia, is the continuation of the tendon.
Activation Maneuver
Flexion of the thigh and extension of the knee activate the muscle. (The rectus femoris crosses the hip and knee joints.)
EMG Needle Insertion
Insert the needle into the anterior thigh midway between the anterior superior iliac spine and the patella.
Pitfalls
There are no pitfalls. If the needle is improperly inserted, it will still be in muscles supplied by the femoral nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the femoral nerve, posterior division of the lumbar plexus, or L2, L3, L4 roots.
Anatomical Illustrations
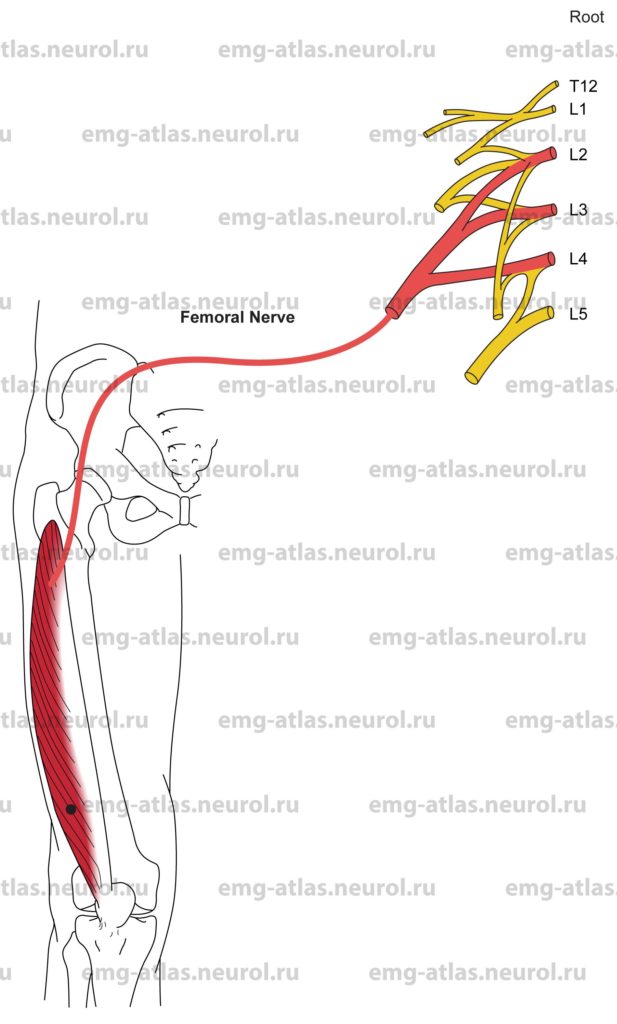
Vastus Lateralis
Innervation
Innervation is via the femoral nerve, posterior division of the lumbar plexus, and roots L2, L3, L4.
Origin
The vastus lateralis originates from the intertrochanteric line, inferior border of the greater trochanter, gluteal tuberosity, and linea aspera of the femur.
Insertion
Insertion is at the tubercle of the tibia via the quadriceps tendon.
Activation Maneuver
Extension of the knee activates the muscle. (Instruct the supine patient to press the knee down into the bed while lifting the heel of the foot off the bed.)
EMG Needle Insertion
Insert the needle into the anterolateral thigh 8-10 cm above the patella.
Pitfalls
If the needle is inserted too posteriorly, it may be in the biceps femoris short head, which is supplied by the peroneal division of the sciatic nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the femoral nerve, posterior division of the lumbar plexus, or L2, L3, L4 roots.
Anatomical Illustrations
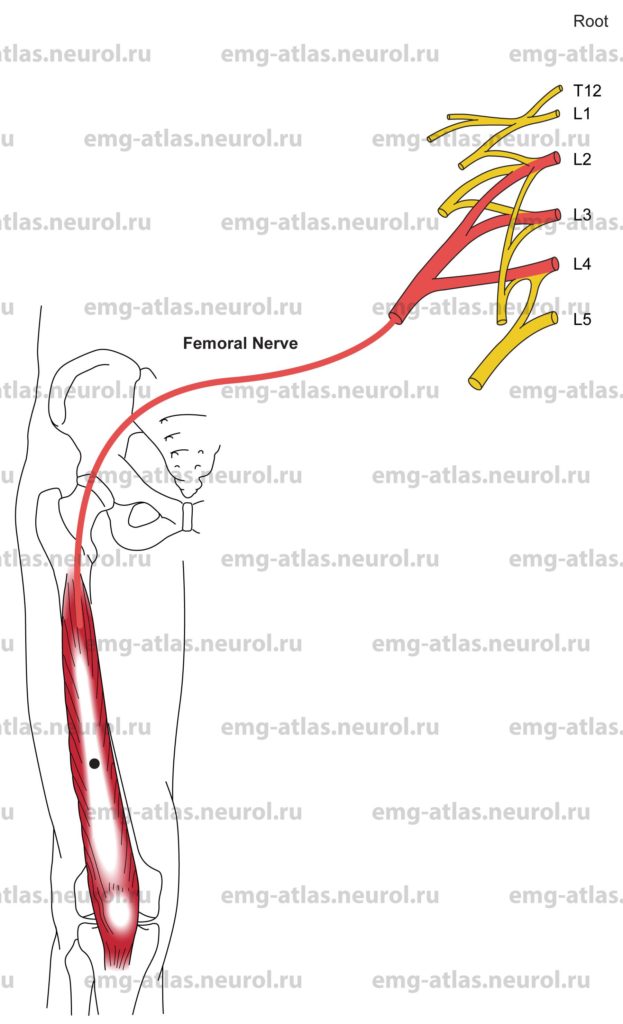
Vastus Intermedius
Innervation
Innervation is via the femoral nerve, posterior division of the lumbar plexus, and roots L2, L3, L4.
Origin
The vastus intermedius originates at the anterior and lateral surfaces of the upper two-thirds of the femoral shaft.
Insertion
Insertion is at the tubercle of the tibia via the quadriceps tendon.
Activation Maneuver
Extension of the knee activates the muscle. (Instruct the supine patient to press the knee down into the bed while lifting the heel of the foot off the bed.)
EMG Needle Insertion
Insert the needle into the anterior thigh midway between the anterior superior iliac spine and the patella. This muscle lies deep to the rectus femoris.
Pitfalls
There are no pitfalls. If the needle is improperly inserted, it will still be in muscles supplied by the femoral nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the femoral nerve, posterior division of the lumbar plexus, or L2, L3, L4 roots.
Anatomical Illustrations
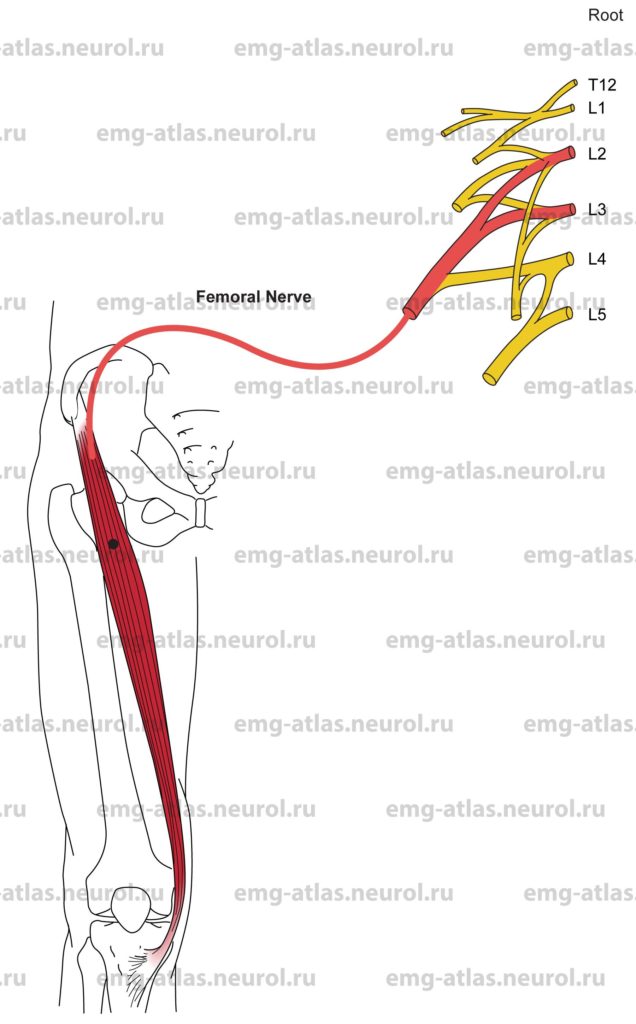
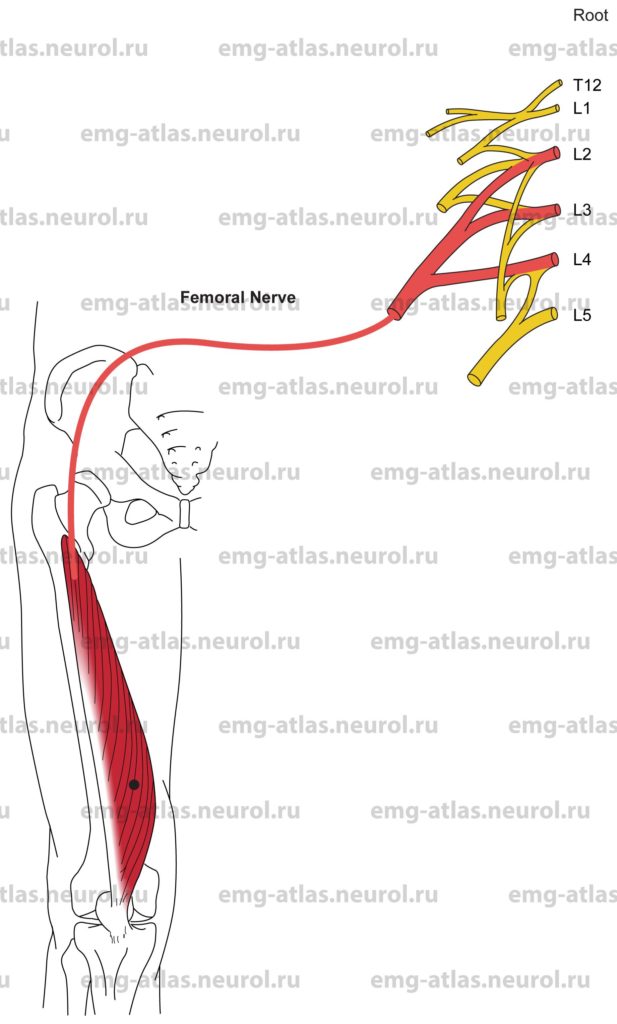
Vastus Medialis
Innervation
Innervation is via the femoral nerve, posterior division of the lumbar plexus, and roots L2, L3, L4.
Origin
The vastus medialis originates from the intertrochanteric line, spiral line, linea aspera, medial supracondylar line of the femur, and the tendons of the adductor longus and magnus.
Insertion
Insertion is at the tubercle of the tibia via the quadriceps tendon.
Activation Maneuver
Extension of the knee activates the muscle. (Instruct the supine patient to press the knee down into the bed while lifting the heel of the foot off the bed.)
EMG Needle Insertion
Insert the needle into the anteromedial thigh 5-7 cm above the patella.
Pitfalls
If the needle is inserted too superiorly and medially, it may be in the adductor magnus, which is supplied by the obturator and sciatic nerves.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the femoral nerve, posterior division of the lumbar plexus, or L2, L3, L4 roots.