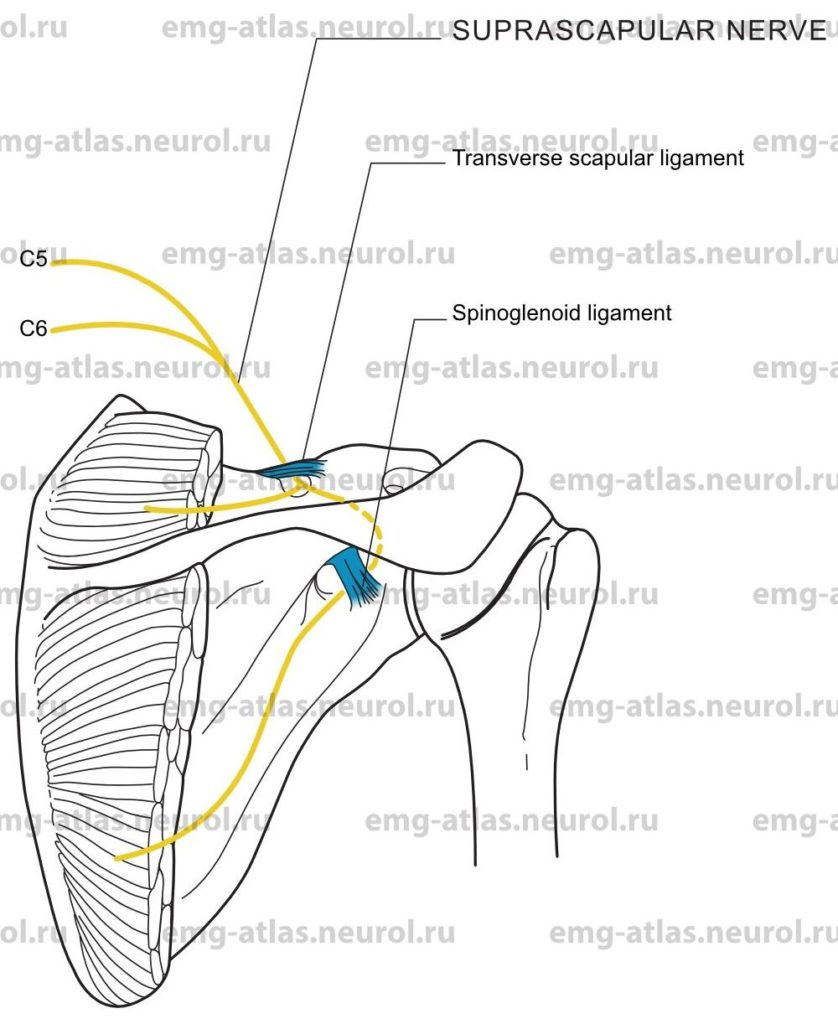
Diagram of the suprascapular nerve (posterior view) to the supraspinatus and infraspinatus muscles.
Fibers to the suprascapular nerve are derived from the fifth and sixth cervical roots (Gray’s Anatomy, 1995). Occasionally, the nerve is derived solely from the fifth or from the fifth and fourth cervical roots (Sunderland, 1968). The nerve arises from the upper trunk of the brachial plexus and passes obliquely outward beneath the trapezius and omohyoid muscles to reach the suprascapular notch of the scapula. This notch is bridged by the superior transverse scapular ligament to form an osseofibrous foramen through which the suprascapular nerve passes to enter the supraspinous fossa. In the fossa, the nerve lies beneath the supraspinatus muscle, which it innervates.
The nerve then continues around the curved free lateral border of the spine of the scapula to reach the spinoglenoid notch. This notch is covered by the inferiortransverse scapular (or spinoglenoid) ligament, which may also form an osseofibrous foramen through which the suprascapular nerve passes to enter the infraspinous fossa. In this fossa, the nerve supplies the infraspinatus muscle. One of the most important uses of the supraspinatus-and infraspinatus muscles is the protection they afford to the shoulder joint; the supraspinatus supports it above and prevents displacement of the head of the humerus upward, while the infraspinatus (and teres minor) protect it posteriorly and prevent dislocation backward.
Suprascapular Nerve Lesion
Etiology
Trauma to the shoulder, fractures of the scapula or humerus, and penetrating wounds can cause direct nerve injury (Hadley et al., 1986).
Entrapment at the suprascapular notch of the scapula, or rarely at the spinoglenoid notch (Aiello et al., 1982), can cause a suprascapular nerve lesion.
Neuralgic amyotrophy (brachial plexopathy) is causative.
General Comments
Trauma often results in combined lesions of the suprascapular nerve and the upper trunk of the brachial plexus (Sunderland, 1968).
Clinical Features
The shoulder pain is usually described as a deep, dull ache located posterolaterally in the shoulder.
There is wasting of the supraspinatus and infraspinatus muscles.
Initiation of abduction of the arm may be difficult, and there may be weakness during external rotation of the humerus. The deltoid and teres minor usually compensate for the loss of the supraspinatus and infraspinatus muscles, respectively.
There is no sensory loss.
Electrodiagnostic Strategy
Demonstrate neurogenic EMG changes in the supraspinatus and infraspinatus muscles.
EMG of the nonsuprascapular innervated C5, C6 muscles may be necessary to exclude radiculopathy or coexisting upper trunk lesion.
Perform nerve conduction studies to exclude neuralgic amyotrophy.
Anatomical Illustrations
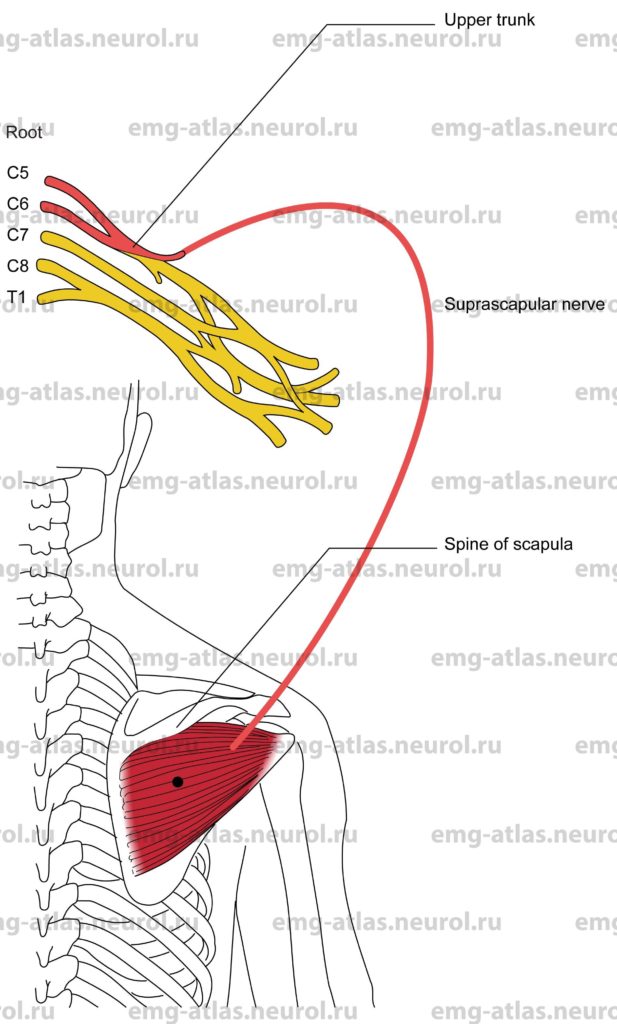
Infraspinatus
Innervation
Innervation is via the suprascapular nerve, upper trunk, and roots C5, C6.
Origin
The infraspinatus originates in the infraspinous fossa of the scapula.
Insertion
Insertion is at the greater tuberosity of the humerus.
Activation Maneuver
External rotation of the humerus activates the muscle.
EMG Needle Insertion
Insert the needle into the infraspinous fossa 2–4 cm below the medial one-third of the spine of the scapula.
Pitfalls
If the needle is inserted too laterally or superficially, it may be in the posterior deltoid, which is supplied by the axillary nerve. Additionally, the trapezius (which is supplied by the spinal accessory nerve) and the latissimus dorsi (supplied by the thoracodorsal nerve) may each lie superficial to the upper and lower margins of the infraspinatus muscle, respectively.
If the needle is placed too caudad, it may be in the teres minor (which is supplied by the axillary nerve) or, rarely, the teres major (supplied by the subscapular nerve).
Clinical Comments
Needle examination may show neurogenic changes when injury to the suprascapular nerve produces axonal loss.
Needle examination may also show neurogenic changes in lesions of the upper trunk and the C5, C6 including Erb’s palsy.
Anatomical Illustrations
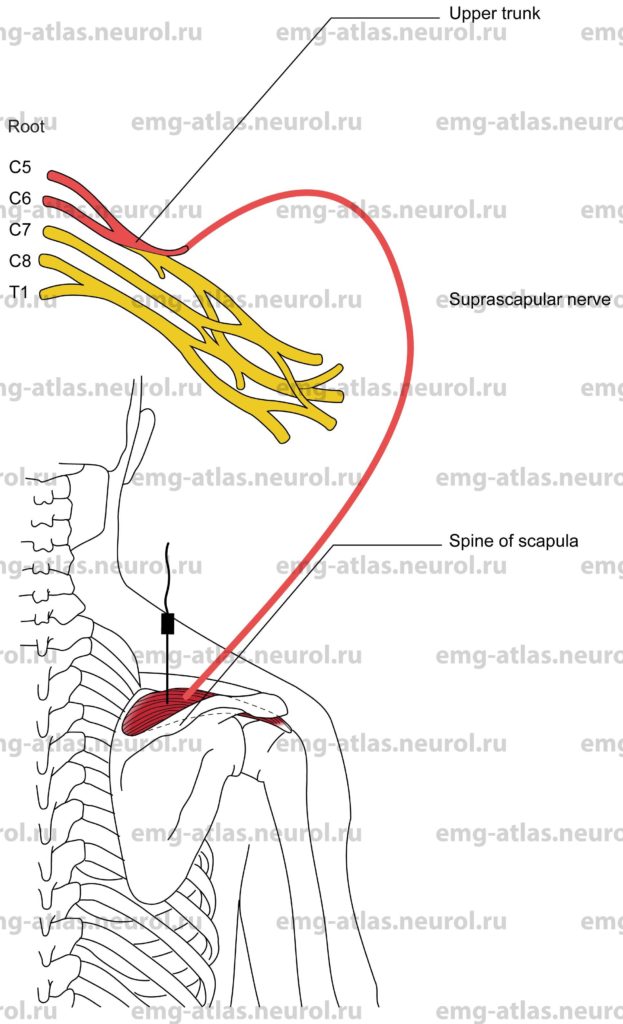
Supraspinatus
Innervation
Innervation is via the Suprascapular nerve, upper trunk, and roots C5, C6.
Origin
The supraspinatus originates in the supraspinous fossa of the scapula.
Insertion
Insertion is at the greater tuberosity of the humerus.
Activation Maneuver
Initiation of abduction of the arm activates the muscle.
EMG Needle Insertion
Insert the needle into the supraspinous fossa just above the spine of the scapula (the lateral margin of the spine is usually easier to palpate). Direct the needle to the bone and then retract slightly.
Pitfalls
If the needle is inserted too superficially, it will be in the trapezius muscle, which is supplied by the spinal accessory nerve and C3 and C4 spinal nerves.
Pneumothorax following supraspinatus EMG needle examination has been reported in the literature (Reinstein et al., 1987).
Clinical Comments
Needle examination may show neurogenic changes when injury to the Suprascapular nerve produces axonal loss.
Needle examination may also show neurogenic changes in lesions of the upper trunk and C5, C6 roots, including Erb’s palsy.