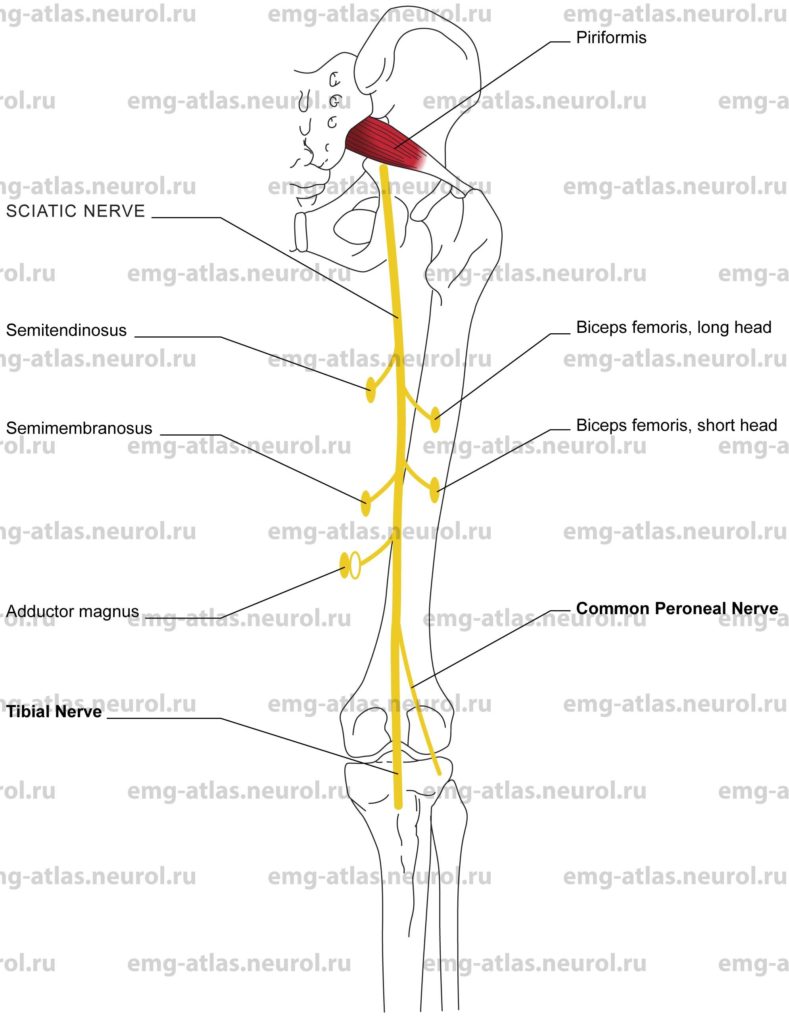
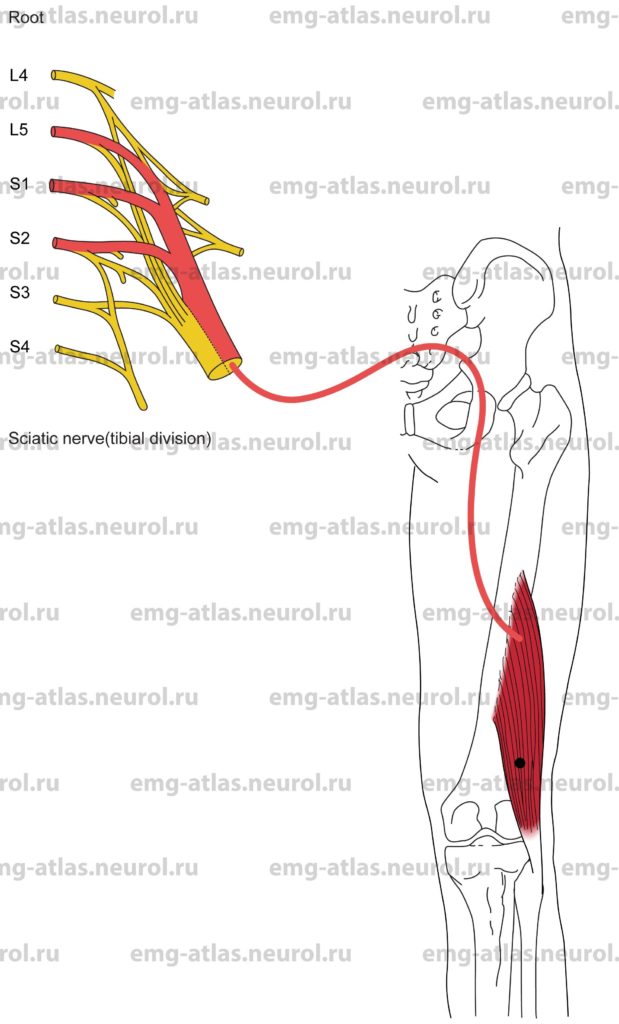
Diagram of the sciatic nerve (posterior view) and its branches. NOTE: The white oval signifies that a muscle receives part of its innervation from another peripheral nerve.
The sciatic nerve is a continuation of the upper, larger cord of the sacral plexus and is formed by the lumbosacral trunk (L4, L5) and the first, second, and part of the third sacral ventral rami (Gray’s Anatomy, 1995). It is the broadest nerve of the human body (2 cm at its origin) and is composed of independent tibial and common peroneal divisions that are usually united as far as the lower part of the thigh, although simple dissection reveals the double structure. In about 10% of cases, the two divisions remain distinct from the outset. The sciatic nerve leaves the pelvis via the greater sciatic foramen below the lower margin of the piriformis muscle and descends between the greater trochanter of the femur and ischial tuberosity along the back of the thigh. Just above the popliteal fossa it separates into its two terminal divisions.
In the gluteal region (after emerging below the piriformis), the nerve is deep to the gluteus maximus. On leaving the gluteal region, the nerve continues down the midline of the thigh closely related to the shaft of the femur. Muscular branches are given to the biceps femoris (the short head is supplied by peroneal division and the long head by tibial division), semitendinosus, semimembranosus, and the ischiocondylar part of the adductor magnus. Articular branches supply the hip joint.
Although the sciatic nerve, or its branches, may be involved by penetrating injuries at any level, there are regions where the nerve is prone to certain types of injury. Anatomical features of particular clinical significance are found in the pelvis (see Chapter 14), the gluteal region, and the thigh (Sunderland, 1968). On leaving the pelvis, the nerve may rarely be entrapped by the piriformis muscle (piriformis syndrome). In the gluteal region the sciatic nerve is at risk because the buttock is a common site for therapeutic injections. The nerve is also intimately related to the hip joint and may be involved with injuries to that joint. Damage may also occur during operations on the hip joint or femur. In the thigh, the nerve may be injured during fractures of the femur or compressed against the firm edge of a seat.
Sciatic Nerve Lesion
Etiology
Tumors and metastatic lesions can cause a sciatic nerve lesion.
Trauma, including hip fracture or dislocation, or more distal fractures of the femur can cause a sciatic nerve lesion.
A traction injury can occur during orthopedic or other surgical manipulation common during hip joint replacement).
Radiation therapy (usually related to radiation plexopathy) is causative.
Compression injury can occur in the gluteal region. As the nerve appears from beneath the gluteus maximus, it is relatively superficial and may be compressed when seated on a firm surface. Common peroneal fibers are maximally or exclusively affected (Sunderland, 1968).
Entrapment by the piriformis muscle (piriformis syndrome) can cause a sciatic nerve lesion.
Intramuscular injections can cause a sciatic nerve lesion. The nerve may be damaged by the needle, by sclerosing or toxic agents, or later by scarring that follows the tissue reaction (Sunderland, 1968).
General Comments
Malignant infiltration usually involves the nerve roots contributing to the formation of the sciatic nerve in the pelvis. It gives rise to painful and slowly progressive paralysis unilaterally (Kimura, 1989).
Radiation injury causes very slowly progressive painless leg weakness.
There is a greater vulnerability of the common peroneal fibers to most injuries of the sciatic nerve. This may be related to various factors, including the more exposed position of the peroneal division in the thigh, and to the poorer blood supply (less nutrient arteries). In addition, the size, number, and disposition of the funiculi may predispose the peroneal division to injury because it is composed of fewer and larger bundles with less connective tissue than the tibial division. Peroneal fibers are also securely fixed at both the sciatic notch and the neck of the fibula and therefore subjected to greater stretch (Sunderland, 1968).
Clinical Features
Weakness or wasting involves the hamstring muscles as well as the muscles supplied by the common peroneal and tibial nerves.
Numbness occurs over the lateral half of the leg and the entire foot.
The Achilles stretch reflex is absent or reduced.
Electrodiagnostic Strategy
Use nerve conduction studies to confirm a lesion involving the tibial and common peroneal fibers (low amplitude or unelicitable sensory responses from sural and superficial peroneal nerves, low amplitude or unelicitable motor responses from tibial and peroneal nerves).
Demonstrate neurogenic EMG needle examination (i.e., spontaneous activity, abnormal motor unit potentials, and abnormal recruitment) in muscles supplied by the sciatic nerve (hamstrings) and muscles supplied by the common peroneal and tibial nerves.
Use needle EMG to exclude lumbosacral radiculopathies. Radiculopathies produce neurogenic findings in paraspinal muscles as well as in limb muscles; peripheral nerve injury never does so because the peripheral nerve is formed by the ventral rami whereas the paraspinal muscles are innervated by the posterior rami (Wilbourn, 1985).
Anatomical Illustrations
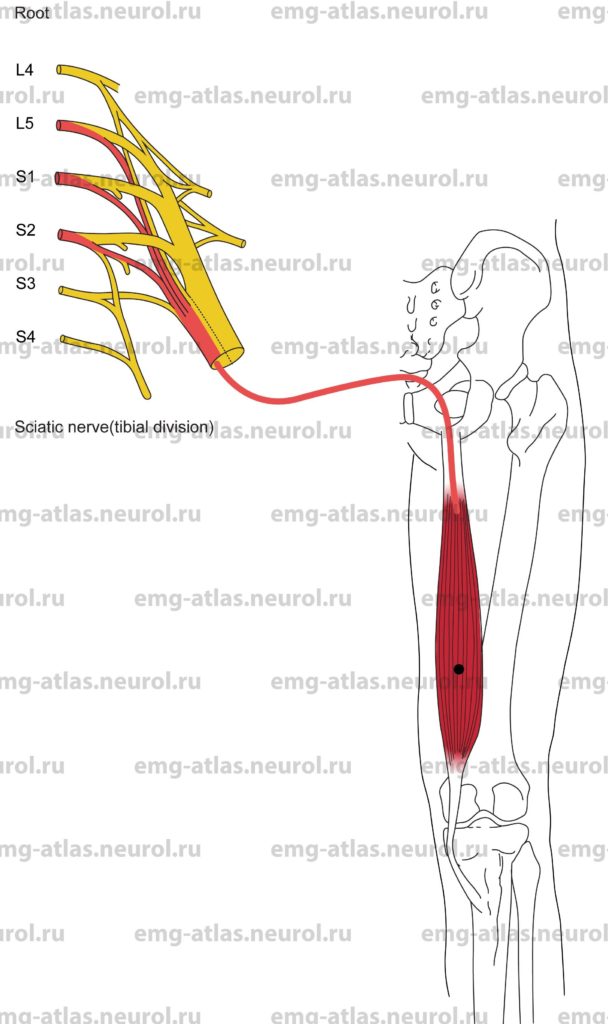
Semitendinosus
Innervation
Innervation is via the sciatic nerve (tibial division), sacral plexus, and roots. L5, S1, S2.
Origin
The semitendinosus originates at the ischial tuberosity.
Insertion
Insertion is at the upper part of the medial surface of the shaft of the tibia.
Activation Maneuver
Flexion of the knee activates the muscle. Note: The «hamstrings» cross both hip and knee joints, integrating extension at the hip with flexion of the knee. In addition, the semitendinosus can act as a medial rotator of the leg.
EMG Needle Insertion
Insert the needle one-third to midway along a line connecting the semitendinosus tendon (easily palpable as it forms the proximal medial margin of the popliteal fossa) with the ischial tuberosity.
Pitfalls
There are no pitfalls. If the needle is inserted too laterally, it may be in the biceps femoris long head, which is also supplied by the tibial division of sciatic nerve and roots L5, S1, and S2. If the needle is inserted too medially, it may be in the semimembranosus (also the tibial division of the sciatic nerve and root L5, S1, S2).
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the tibial division of the sciatic nerve, sacral plexus, and roots L5, S1, or S2.
Anatomical Illustrations
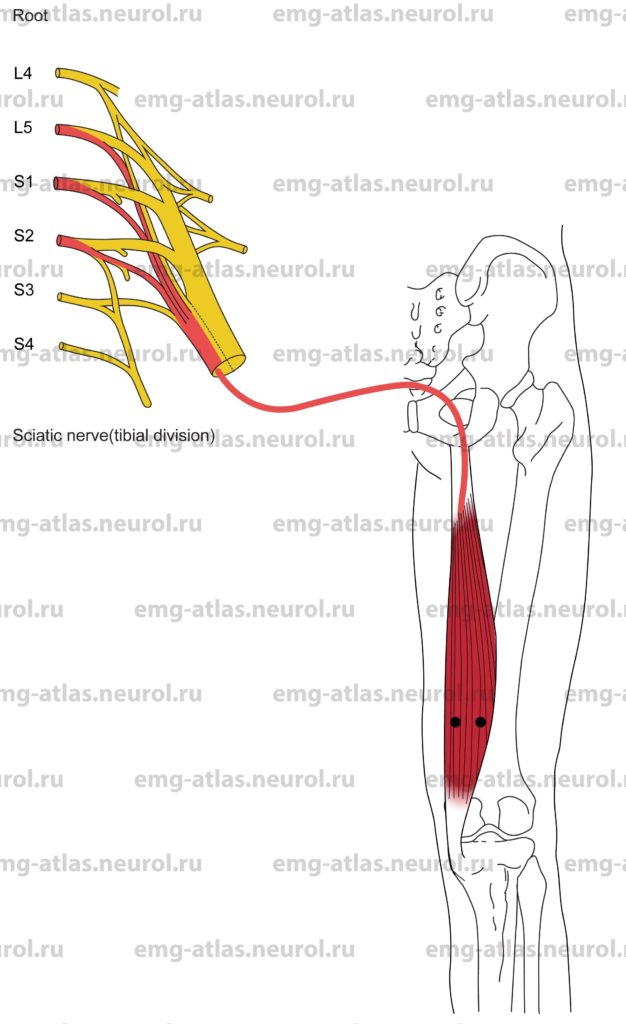
Semimembranosus
Innervation
Innervation is via the sciatic nerve (tibial division), sacral plexus, and roots L5, S1, S2.
Origin
The semimembranosus originates at the ischial tuberosity.
Insertion
Insertion is at the medial condyle of the tibia (major insertion); it also inserts on the medial shaft of the tibia and the fascia over the popliteus and contributes to an expansion that inserts on the lateral femoral condyle.
Activation Maneuver
Flexion of the knee activates the muscle. Note: The «hamstrings» cross both hip and knee joints, integrating extension at the hip with flexion of the knee. In addition, the semimembranosus can act as a medial rotator of the leg.
EMG Needle Insertion
Palpate the semitendinosus tendon in the proximal popliteal fossa. Insert the needle on either side of the semitendinosus tendon.
Pitfalls
If the needle is inserted too laterally, it may be in the biceps femoris short head, which is supplied by the peroneal division of the sciatic nerve and roots L5, S1, S2.
If the needle is inserted too medially and proximally, it may be in the adductor magnus or gracilis. The adductor magnus is supplied by the obturator nerve and the tibial division of the sciatic nerve (L2-L4 roots), while the gracilis receives innervation from the obturator nerve (L2-L3 roots).
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the tibial division of the sciatic nerve, sacral plexus, and roots L5, S1 or S2.
Anatomical Illustrations
Biceps Femoris (Long Head)
Innervation
Innervation is via the sciatic nerve (tibial division). Sacral plexus, and roots L5, S1, S2.
Origin
The long head of the biceps femoris originates at the ischial tuberosity.
Insertion
Insertion is at the head of the fibula.
Activation Maneuver
Flexion of the knee activates the muscle. Note: The «hamstrings» cross both hip and knee joints, integrating extension at the hip with flexion of the knee. In addition, the biceps femoris can act as a latera rotator of the leg.
EMG Needle Insertion
Insert the needle one-third to midway along a line connecting the fibular head with the ischial tuberosity.
Pitfalls
If the needle is inserted too distally, it may be in the short head of the biceps femoris, which is supplied by the peroneal division of the sciatic nerve and roots L5, S1, S2 (at the midthigh, the fibers of the short head are narrow and deep).
If the needle is inserted too laterally, it may be in the vastus lateralis, which is supplied by the femoral nerve (L2-L4 roots). If the needle is inserted too medially, it may be in the semitendinosus, which is also supplied by the tibial division of the sciatic nerve (L5, S2 roots).
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the tibial division of the sciatic nerve, sacral plexus, and roots L5, S1, or S2.
Anatomical Illustrations
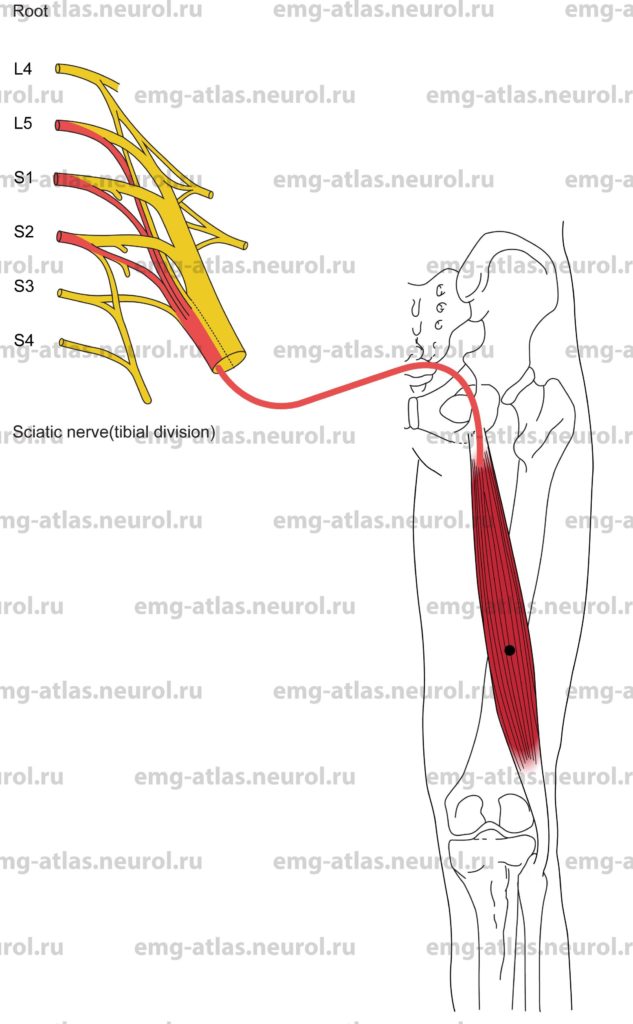
Biceps Femoris (Short Head)
Innervation
Innervation is via the sciatic nerve (peroneal division), sacral plexus, and roots L5, S1, S2.
Origin
The short head of the biceps femoris originates at the lateral lip of the linea aspera on the posterolateral surface of the shaft of the femur and from the lateral intermuscular septum.
Insertion
Insertion is at the head of the fibula.
Activation Maneuver
Flexion of the knee activates the muscle. The short head of the biceps femoris does not cross the hip joint; it cannot contribute to hip extension, but it can act as a lateral rotator of the leg.
EMG Needle Insertion
Palpate the tendon of the long head of the biceps femoris in the popliteal fossa. Insert the needle just medial to the tendon.
Pitfalls
If the needle is inserted too laterally it may penetrate the long head of the biceps femoris, which is supplied by the tibial division of the sciatic nerve (roots L5, S1, S2). If the needle is inserted too medially, it may be in the semimembranosus, which is supplied by the tibial division of the sciatic nerve (roots L5, S1, S2).
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the peroneal division of the sciatic nerve, sacral plexus, and L5, S1, or S2 roots. This is the only muscle in the thigh innervated by the peroneal division of the sciatic nerve.
This muscle is of great importance in the electrodiagnostic evaluation of peroneal nerve lesions because it is crucial in defining the proximal extent of the lesion. If neurogenic EMG changes are present in this muscle, the lesion must be at’or proximal to the midthigh (Wilbourn, 1986).