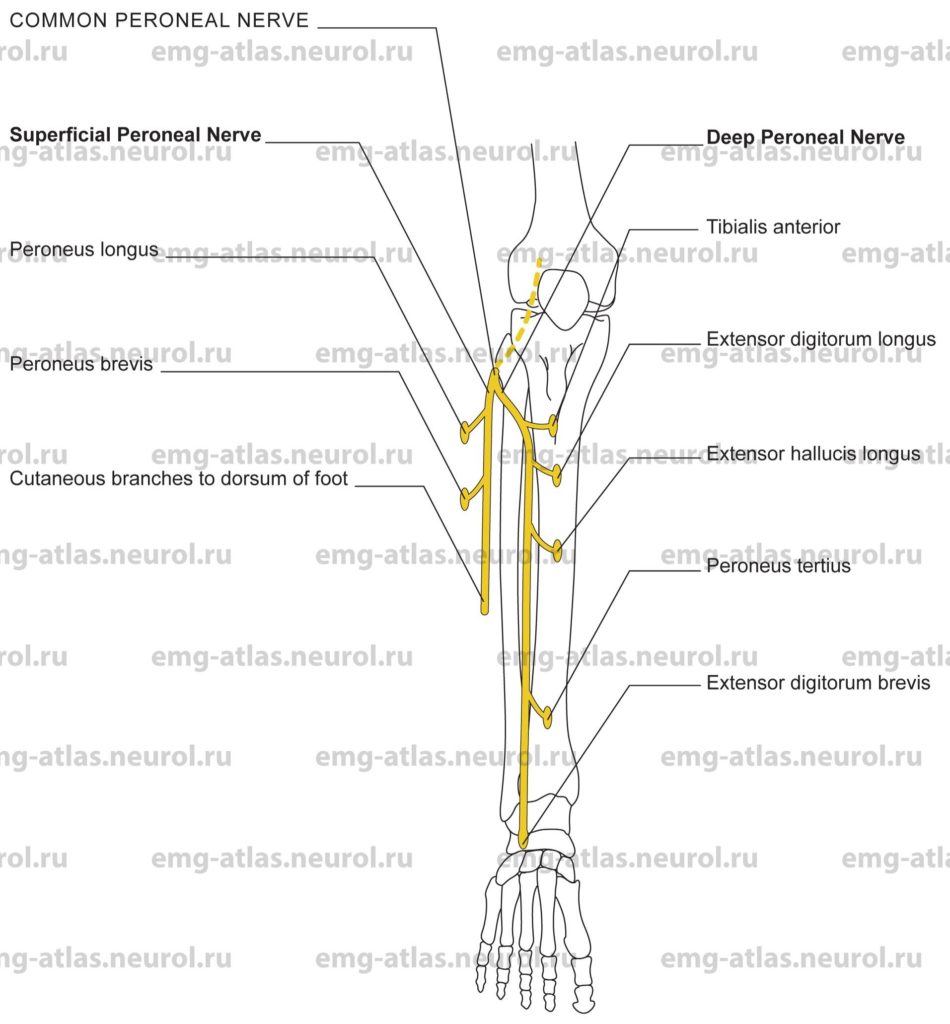
Diagram of the common peroneal nerve (anterior view) and its branches.
The common peroneal nerve is derived from the fourth and fifth lumbar and first and second sacral ventral rami (Gray’s Anatomy, 1995). It descends obliquely along the lateral side of the popliteal fossa, medial to the tendon of the biceps femoris as far as the attachment of the latter to the head of the fibula. It gives off two cutaneous branches, the lateral sural nerve (lateral cutaneous nerve of the calf) and the sural communicating nerve. The former supplies the skin of the anterior, lateral, and posterior aspects of the leg, the latter descends medially to join the sural nerve in the furrow between the two gastrocnemius muscles. Articular branches in the fossa supply the knee joint. The nerve then curves laterally around the neck of the fibula, passing between the two heads of the peroneus longus before dividing into its two terminal branches: the superficial peroneal and the deep peroneal nerves. At the neck of the fibula, the nerve is flattened and superficial and can be easily rolled against the bone (Sunderland, 1968).
The deep peroneal nerve (also known as the anterior tibial nerve) passes medially deep to the extensor digitorum longus and in front of the interosseous membrane. It descends on the interosseous membrane to the ankle, dividing there into lateral and medial terminal branches. Muscular branches in the leg supply the tibialis anterior, extensor digitorum longus, extensor hallucis longus, and peroneus tertius. The lateral terminal branch runs laterally on the dorsum of the foot to supply the extensor digitorum brevis. It also gives off interosseous branches to the tarsal and metatarsophalangeal joints and to the second dorsal interosseous muscle. The medial terminal branch runs distally on the dorsum of the foot and terminates in the first interspace where it provides cutaneous innervation to the skin on the contiguous sides of the great and second toes. It also gives off branches to the tarsal and metatarsophalangeal joints and the first dorsal interosseous muscle.
The superficial peroneal nerve turns downward between the peroneus longus and the extensor digitorum longus and emerges from between them at the mid to lower third of the leg, where it divides into lateral and medial terminal branches. In its course it supplies the peroneus longus and the peroneus brevis. The two terminal branches are cutaneous. The medial supplies the medial aspect of the dorsum of the foot, medial side of the great toe, and the contiguous sides of the second and third toes. The lateral supplies the lateral aspect of the dorsum of the foot and adjoining sides of the third and fourth, and fourth and fifth toes.
While the common peroneal nerve, or its branches, may be involved by penetrating injuries at any level, there are regions where the nerve is prone to certain types of injury. In the popliteal fossa, the nerve is intimately related to the knee joint as it curves laterally to reach the head of the fibula. In this position the nerve may be stretched or torn in medial (adduction) dislocations of the knee joint (Sunderland, 1968). At the head and neck of the fibula, the nerve is superficial and may be damaged by fractures of the fibula, blows to the lateral side of the knee, superficial lacerations, pressure from improperly applied casts, compression or ischemia resulting from habitual leg crossing, or compression against any hard surface. Emaciation and weight loss are also conditions that predispose the nerve to injury.
Common Peroneal Mononeuropathy at the Knee
Etiology
Injury to the common peroneal nerve or its branches as the nerve winds around the head and neck of the fibula can cause common peroneal mononeurophathy at the knee.
The condition is usually traumatic in origin due to compression, traction, or laceration.
General Comments
Mononeuropathy at the knee is common.
Compression can cause nerve dysfunction by both a single episode and by repeated episodes (e.g., habitual leg crossing).
Unilateral symptoms are more common, but bilateral asymmetrical involvement is often seen in patients who are habitual leg crossers, are emaciated and bedridden, or have sustained nerve infarcts from vasculitis (Wilbourn, 1986).
Clinical Features
There is weakness of foot dorsiflexion (“foot drop”). This is the chief complaint in almost all patients.
Weakness occurs during extension of the toes.
Weakness of foot eversion can occur (due to involvement of the superficial peroneal fibers that supply the peroneus longus and brevis). Note: foot eversion may be normal in some patients with common peroneal mononeuropathy at the knee.
Loss of sensation or numbness can occur over the anterolateral part of the leg and the dorsum of the foot.
Electrodiagnostic Strategy
Use nerve conduction studies to confirm a focal lesion of common peroneal motor and sensory fibers at the fibular head. Routine techniques are available that can identify conduction abnormalities across the fibular head (Katirji and Wilbourn, 1984; Wilbourn, 1986).
Perform EMG needle examination in muscles innervated by both the deep peroneal nerve and the superficial peroneal nerve. In common peroneal mononeuropathy associated with loss of motor fibers, EMG will show neurogenic changes (i.e., spontaneous activity, abnormal motor unit potentials, and abnormal recruitment).
If EMG is abnormal in muscles innervated by the common peroneal nerve, study the biceps femoris (short head) to define the proximal extent of the lesion (i.e., neurogenic changes in this muscle suggest a sciatic mononeuropathy with disproportionate involvement of common peroneal fibers).
Exclude s5 radiculopathy as the etiology of foot drop (perform a needle examination in the tensor fasciae latae, gluteus medius, and lumbosacral paraspinal muscles).
Anatomical Illustrations
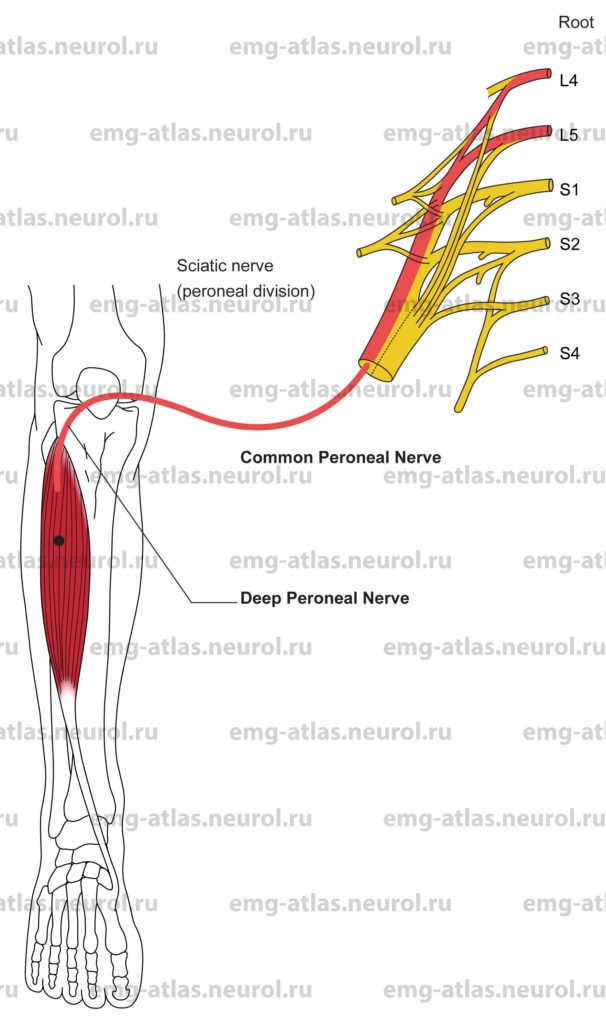
Tibialis Anterior
Innervation
Innervation is via the deep peroneal nerve, common peroneal nerve, peroneal division of the sciatic nerve, sacral plexus, and roots L4, L5.
Origin
The tibialis anterior originates from the lateral condyle of the tibia and the proximal half of the lateral surface of the shaft of the tibia.
Insertion
Insertion is at the medial cuneiform bone and adjoining part of the base of the first metatarsal bone.
Activation Maneuver
Dorsiflexion of the foot activates the muscle.
EMG Needle Insertion
Insert the needle just lateral to the proximal half of the shaft of the tibia (the muscle is superficial and readily palpable lateral to the tibia).
Pitfalls
There are no pitfalls. If the needle is inserted too laterally or deeply, it will be in the extensor digitorum longus, which is also innervated by the deep peroneal nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the deep peroneal nerve, common peroneal nerve, peroneal division of the sciatic nerve, sacral plexus, or L4, L5 roots.
In the evaluation of severe «foot drop» always examine L5 muscles that are not supplied by the common peroneal nerve (i.e., tibialis posterior, flexor digitorum longus, tensor fasciae latae, gluteus medius, or paraspinals) to exclude an L5 radiculopathy. Conversely, these muscles are normal in foot drop due solely to peroneal mononeuropathy.
The tibialis anterior may also contribute to inversion of the foot because its tendon inserts on the medial aspect of the foot.
Anatomical Illustrations
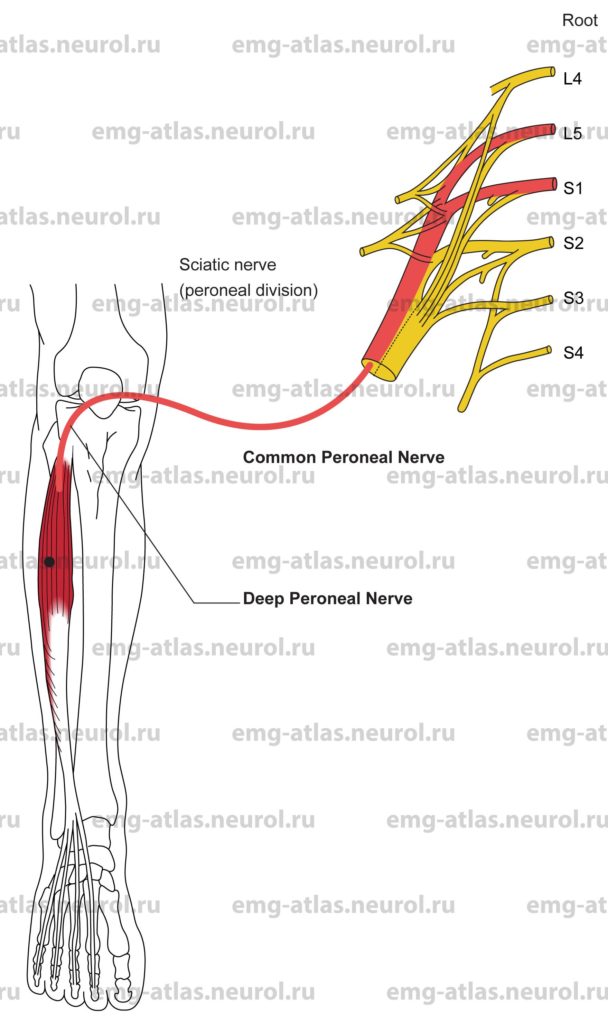
Extensor Digitorum Longus
Innervation
Innervation is via the deep peroneal nerve, common peroneal nerve, peroneal division of the sciatic nerve, sacral plexus, and roots L5, S1.
Origin
The extensor digitorum longus originates from the lateral condyle of the tibia, the proximal three-fourths of the medial surface of the fibula, and the interosseous membrane.
Insertion
Insertion is into the dorsal digital expansion, which also receives contributions from the extensor digitorum brevis, lumbricals, and interosseous muscles. The expansion attaches to the bases of the middle phalanges with collateral slips that attach to the bases of the distal phalanges of the toes.
Activation Maneuver
Extension of the four lateral toes activates the muscles.
EMG Needle Insertion
Insert the needle 6-7 cm distal to the tibial tuberosity and 4-5 cm lateral to the shaft of the tibia. The muscle is superficial in this location, lying between the tibialis anterior and the peroneus longus (Gray’s Anatomy, 1995).
Pitfalls
If the needle is inserted too laterally, it will be in the peroneus longus, which is innervated by the superficial peroneal nerve.
If the needle is inserted too anteriorly, it will be in the tibialis anterior, which is also innervated by the deep peroneal nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the deep peroneal nerve, common peroneal nerve, peroneal division of the sciatic nerve, sacral plexus, or L5, S1 roots.
Anatomical Illustrations
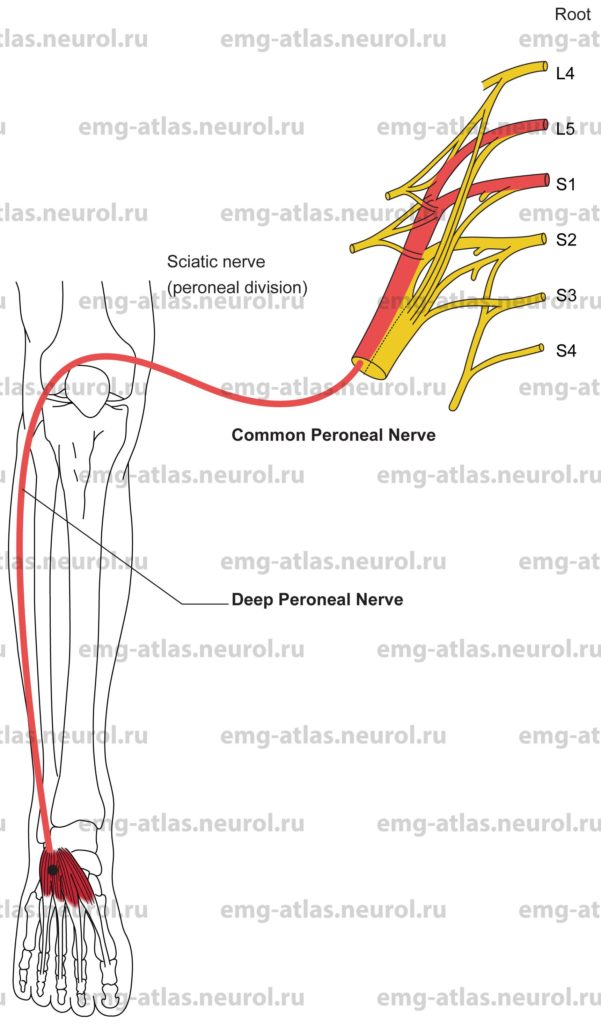
Extensor Hallucis Longus
Innervation
Innveration is via the deep peroneal nerve, common peroneal nerve, peroneal division of the sciatic nerve, sacral plexus, and roots L5, S1.
Origin
The extensor hallucis longus originates from the midportion of the medial surface of the fibula and adjacent interosseous membrane.
Insertion
Insertion is at the base of the distal phalanx of the hallux (great toe).
Activation Maneuver
Extension of the great toe activates the muscle.
EMG Needle Insertion
Insert the needle 7-9 cm proximal to the bimalleolar line of the ankle just lateral to the shaft of the tibia.
Pitfalls
There are no pitfalls. If the needle is inserted too laterally it will be in the peroneus tertius, which is also innervated by the deep peroneal nerve; if the needle is inserted too superficial or too proximal, it may be in the tibialis anterior or extensor digitorum longus, which are also innervated by the deep peroneal nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the deep peroneal nerve, common peroneal nerve, peroneal division of the sciatic nerve, sacral plexus, or L5, S1 roots.
Anatomical Illustrations
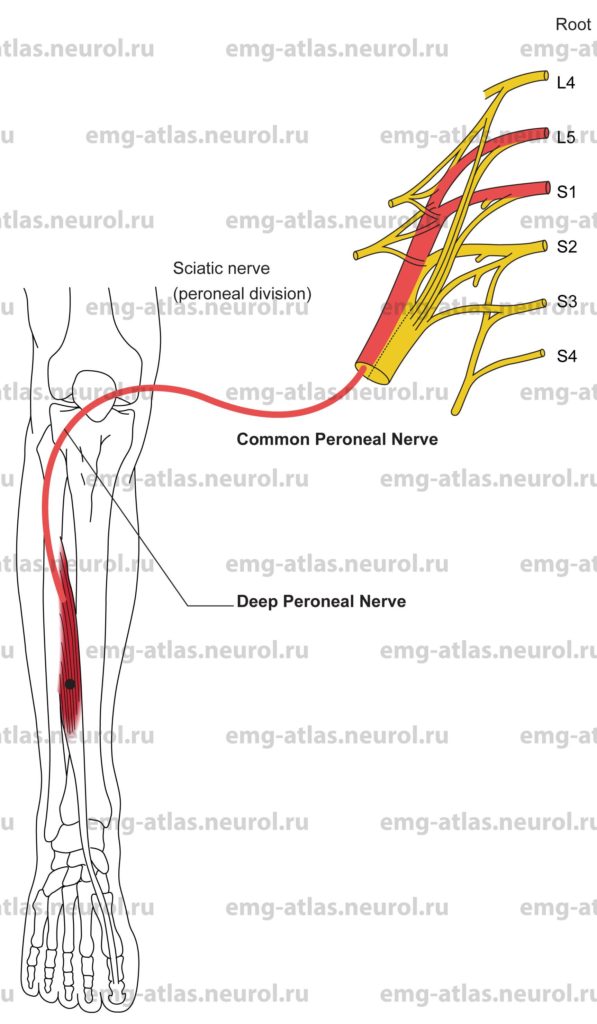
Peroneus Tertius
Innervation
Innervation is via the deep peroneal nerve, common peroneal nerve, peroneal division of the sciatic nerve, sacral plexus, and roots L5, S1.
Origin
The peroneus tertius originates from the distal fourth of the anterior surface of the fibula and the adjacent interosseous membrane.
Insertion
Insertion is at the dorsal surface of the base of the fifth metatarsal bone.
Activation Maneuver
Dorsiflexon and eversion of the foot activate the muscle.
EMG Needle Insertion
Insert the needle 6-8 cm proximal to the bimalleolar line of the ankle and 2-3 cm lateral to the shaft of the tibia.
Pitfalls
There are no pitfalls. If the needle is inserted too laterally, it will encounter the fibula; if it is inserted too anterior, it may penetrate the tendons of the tibialis anterior or extensor digitorum longus or enter the extensor hallucis longus, which is also innervated by the deep peroneal nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the deep peroneal nerve, common peroneal nerve, peroneal division of the sciatic nerve, sacral plexus, or L5, S1 roots.
Anatomical Illustrations
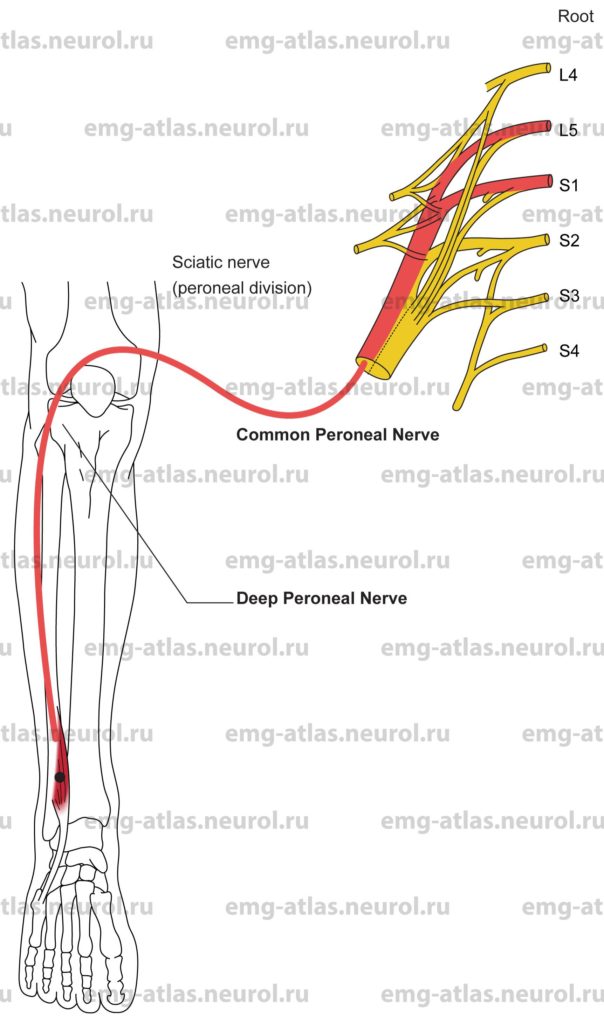
Extensor Digitorum Brevis
Innervation
Innervation is via the deep peroneal nerve, common peroneal nerve, peroneal division of the sciatic nerve, sacral plexus, and roots L5, S1.
In 20%-28% of subjects, an accessory deep peroneal nerve also supplies this muscle (Gutmann, 1993). The accessory deep peroneal nerve is an anomalous motor branch originating from the superficial peroneal nerve. It descends on the lateral aspect of the leg, passes posterior to the lateral malleolus, and proceeds anteriorly to supply the lateral portion of the extensor digitorum brevis.
Origin
The extensor digitorum brevis originates from the anterior and superolateral surfaces of the calcaneus.
Insertion
Insertion is into the dorsal digital expansion, which also receives contributions from the extensor digitorum longus, lumbricals, and interosseous muscles. The expansion attaches to the bases of the middle phalanges with collateral slips that attach to the bases of the distal phalanges of the toes. The extensor digitorum brevis contributes four tendons; three attach to the tendons of the extensor digitorum longus for the second through fourth toes, and one inserts into the base of the proximal phalanx of the hallux; this latter slip is sometimes termed the extensor halluds brew’s.
Activation Maneuver
Extension of the toes activates the muscle.
EMG Needle Insertion
Insert the needle into the small mound of muscle tissue located on the proximal lateral aspect of the dorsum of the foot.
Pitfalls
The muscle may be difficult to examine in patients with peripheral neuropathies or other conditions predisposing to atrophy (e.g., compression from chronically tight shpes).
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the deep peroneal nerve, common peroneal nerve, peroneal division of the sciatic nerve, sacral plexus, or L5, S1 roots.
The extensor digitorum brevis is involved early in length-dependent peripheral neuropathies.
Neurogenic changes on needle examination may reflect chronic compression of the nerve or muscle from tight shoes or high-healed shoes (Dawson et al., 1990).
This muscle is commonly used to record the compound muscle action potential during peroneal nerve conduction studies.
Anatomical Illustrations
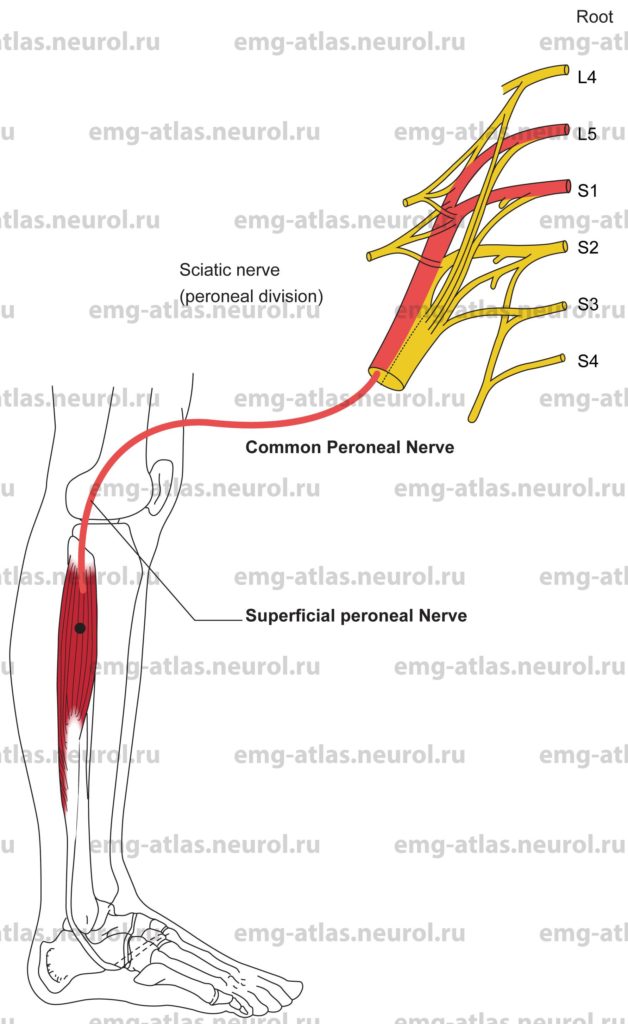
Peroneus Longus
Innervation
Innervation is via the superficial peroneal nerve, common peroneal nerve, peroneal division of the sciatic nerve, sacral plexus, and roots L5, S1.
Origin
The peroneus longus originates from the head and proximal two-thirds of the lateral surface of the fibula.
Insertion
Insertion is at the lateral surface of the base of the first metatarsal bone and the medial cuneiform bone.
Activation Maneuver
Eversion of the foot activates the muscle.
Note: This muscle can also plantar flex the foot because its tendon runs distally behind the lateral malleolus.
EMG Needle Insertion
Insert the needle 5-7 cm below the fibular head along the lateral aspect of the fibula.
Pitfalls
If the needle is inserted too posteriorly, it will be in the soleus or lateral gastrocnemius, which are supplied by the tibial nerve.
If the needle is inserted too anteriorly it, will be in the extensor digitorum longus, which is supplied by the deep peroneal nerve.
To minimize pitfalls, activation of the peroneus longus (i.e., eversion of the foot) should be performed while flexing the toes and slightly dorsiflexing the foot. This will avoid coactivation of the adjacent extensor digitorum longus and lateral gastrocnemius, respectively.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the superficial peroneal nerve, common peroneal nerve, peroneal division of the sciatic nerve, sacral plexus, or L5, S1, roots.
Anatomical Illustrations
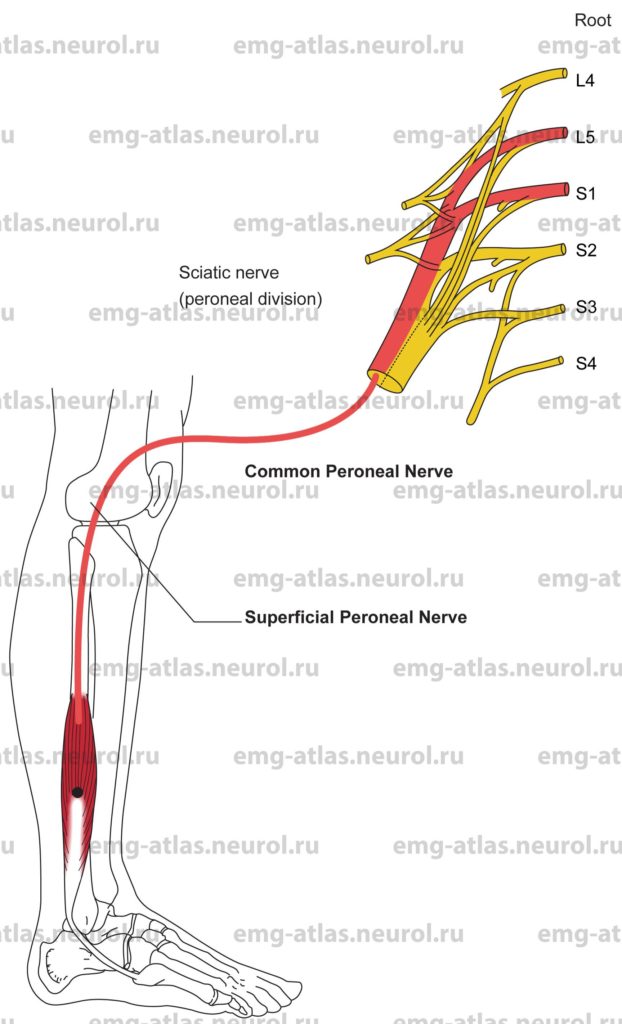
Peroneus Brevis
Innervation
Innervation is via the superficial peroneal nerve, common peroneal nerve, peroneal division of the sciatic nerve, sacral plexus, and roots L5, S1.
Origin
The peroneus brevis originates from the distal two-thirds of the lateral surface of the fibula.
Insertion
Insertion is at the lateral surface of the base of the fifth metatarsal bone.
Activation Maneuver
Eversion of the foot activates the muscle.
Note: This muscle can also plantar flex the foot because its tendon, together with that of the peroneus longus, passes behind the lateral malleolus.
EMG Needle Insertion
Insert the needle 8-10 cm above the lateral malleolus just posterior to the lateral aspect of the fibula.
Pitfalls
If the needle is inserted anterior to the lateral aspect of the fibula, it will be in the peroneus tertius supplied by the deep peroneal nerve.
If the needle is inserted too deeply it will be in the flexor hallucis longus, which is supplied by the tibial nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the superficial peroneal nerve, common peroneal nerve, peroneal division of the sciatic nerve, sacral plexus, or L5, S1 roots.