The subscapular nerves and the thoracodorsal nerve are all branches of the posterior cord of the brachial plexus. The upper and lower subscapular nerves arise from the fifth and sixth cervical nerves, while thoracodorsal nerve arises from the sixth through eighth cervical nerves. The upper and lower subscapular nerves are short and supply the subscapularis and teres major muscles, respectively (Sunderland, 1968).
The subscapularis muscle is of little EMG importance, as it is generally inaccessible to needle examination (it fills the subscapular fossa and terminates in a tendon that inserts on the lesser tuberosity of the humerus). The teres major and latissimus dorsi, however, can be examined during routine EMG evaluation. The nerve to the latissimus dorsi is historically considered as the middle or long subscapular nerve (Sunderland, 1968; Gray’s Anatomy, 1977), more recently renamed the thoracodorsal nerve (Gray’s Anatomy, 1995). The thoracodorsal nerve runs a long, exposed course on the posterior wall of the axilla to reach the deep surface latissimus dorsi. It is intimately related to lymph nodes along its course and may be damaged during surgical procedures on the axilla.
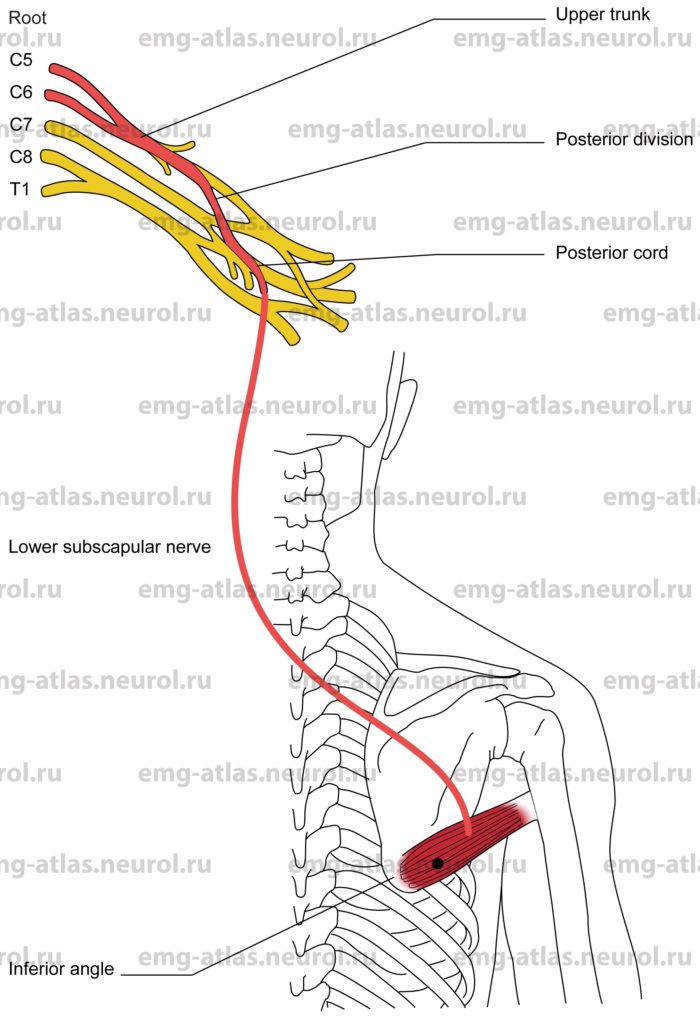
Anatomical Illustrations
Teres Major
A posterior view of the brachial plexus and the lower subscapular nerve is shown in the drawing and photograph.
Innervation
Innervation is via the lower subscapular nerve, posterior cord, upper trunk, and roots C5, C6.
Origin
The teres major originates at the dorsal aspect of the inferior angle scapula.
Insertion
Insertion is at the inner bicipital ridge of the humerus.
Activation Maneuver
Internal rotation and abduction of the humerus activates the muscle. EMG Needle Insertion
Insert the needle along lateral lower border of the scapula (lateral and rostral to the inferior angle).
Pitfalls
If the needle is inserted too caudally or laterally, it may be in the latissimus dorsi. The latissimus at first covers the origin of the teres major and then wraps itself obliquely around its lower border so that its tendon ultimately comes to lie in front of that of the teres major.
If the needle is inserted too rostrally (superiorly), it may be in the teres minor, which is supplied by the axillary nerve.
If the needle is inserted too deeply, it may penetrate the serratus anterior, supplied by the long thoracic nerve.
Clinical Comments
An isolated lesion of the lower subscapular nerve is rare. It is unlikely that weakness limited to the teres major would be clinically detectable.
Neurogenic EMG changes in the teres major may be seen with C5 or C6 radiculopathy.
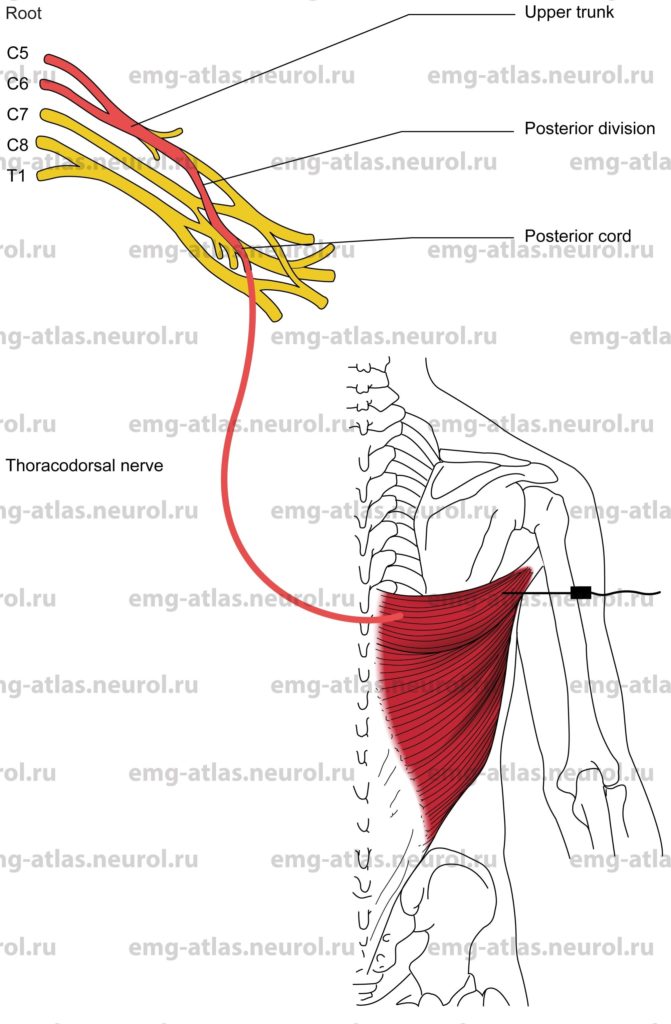
Anatomical Illustrations
Latissimus Dorsi
A posterior view of the brachial plexus and the thoracodorsal nerve is shown in the drawing and photograph.
Innervation
Innervation is via the thoracodorsal nerve (formerly the middle subscapular nerve); posterior cord; upper, middle, and lower trunks; and roots C6, C7, C8.
Origin
The latissimus dorsi originates at the spinous process of the six inferior thoracic vertebrae, the posterior layer of the lumbar fascia (by which it is attached to the spines of the lumbar and sacral vertebrae), and the crest of the ilium.
Insertion
Insertion is at the bicipital groove of the humerus.
Activation Maneuver
Internal rotation, abduction, and extension (drawing the arm backward) of the humerus activates the muscle. EMG Needle Insertion
Insert the needle along posterior axillary fold directly lateral to the inferior angle of the scapula.
Pitfalls
If the needle is inserted too superiorly, it may be in the teres major. The latissimus at first covers the origin of the teres major and then wraps itself obliquely around its lower border so that its tendon ultimately comes to lie in front of that of the teres major.
Clinical Comments
Atrophy and weakness of the latissimus dorsi is not easily detected because wasting is not often noticeable and functions (internal rotation, adduction, and extension) can be executed by other muscles (Sunderland, 1968).
Neurogenic EMG changes in the latissimus dorsi may be seen with C6, C7 or C8 radiculopathy.