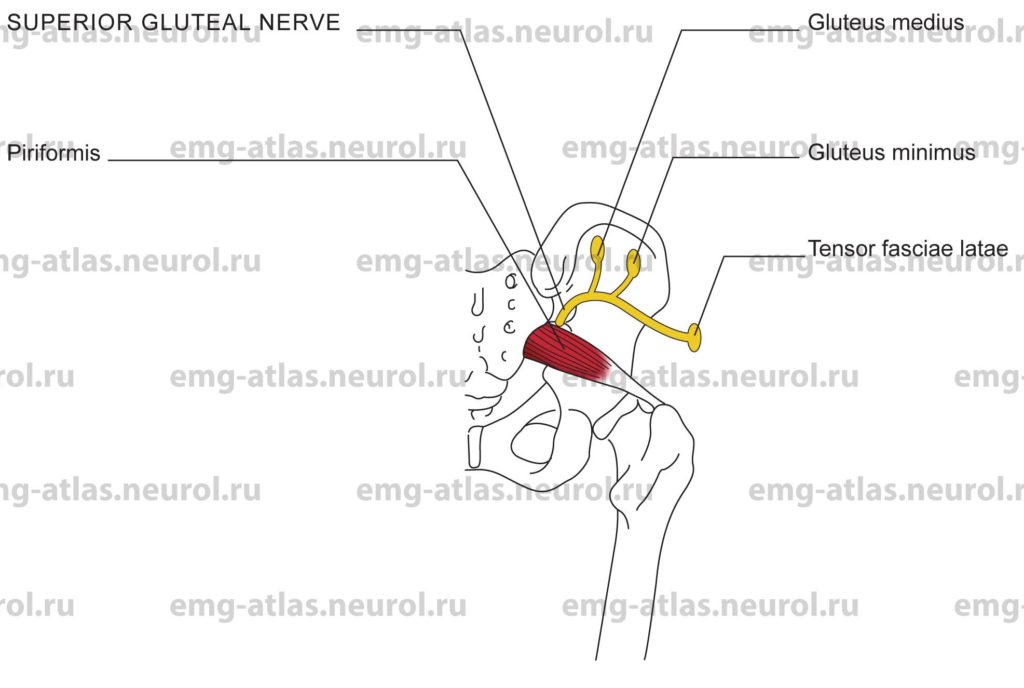
Diagram of the superior gluteal nerve (posterior view) and its branches.
The superior gluteal nerve arises from the posterior branches of the fourth and fifth lumbar and the first sacral ventral rami. It leaves the pelvis via the greater sciatic foremen above the piriformis muscle with the superior gluteal vessels and divides into superior and inferior branches. The superior branch follows the line of origin of the gluteus minimus to supply the gluteus medius. The inferior branch crosses obliquely between the gluteus minimus and gluteus medius, distributing filaments to both of these muscles, before terminating in the tensor fasciae latae.
The gluteus medius and minimus play an essential role in maintaining the trunk upright when the opposite foot is in the swing phase of the gait cycle. In this phase, the weight of the unsupported leg tends to make the pelvis sag downward. This is counteracted by the gluteus medius and minimus of the supporting side, which exert such a powerful traction on the hip bone that the pelvis on the unsupported side is actually raised slightly (Gray’s Anatomy, 1995). This supportive effect of the glutei on the contralateral pelvis depends on preserved innervation to the two muscles and on the normal relationship between the components of the hip joint. When these conditions are not fulfilled, such as in lesions of the superior gluteal nerve, congenital dislocation of the hip, or nonunion fracture of the neck of the femur, the supportive effect of the glutei is abolished and the pelvis sinks on the contralateral foot during its swing phase. This results in a characteristic lurching gait (Trendelenberg’s sign). Paralysis of the gluteus medius and minimus is the most serious muscular disability affecting the hip; paralysis of other muscles acting on the hip joint produces relatively little gait dysfunction.
Anatomical Illustrations
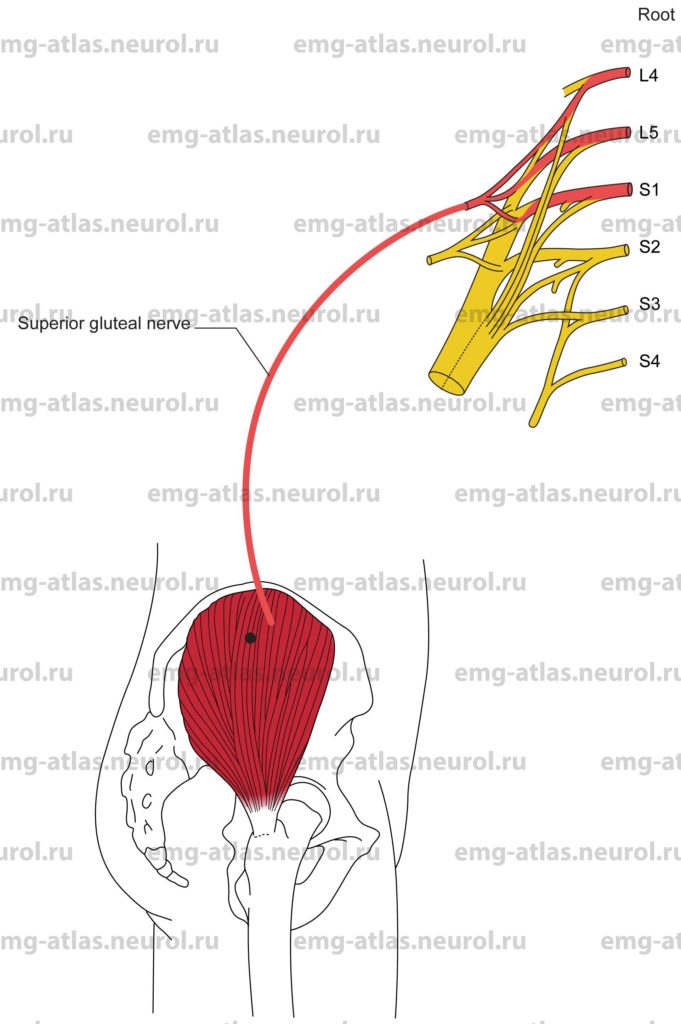
Gluteus Medius
Innervation
Innervation is via the superior gluteal nerve, sacral plexus, and roots L4, L5 S1.
Origin
The gluteus medius originates from the outer surface of the ilium between the iliac crest above and the anterior gluteal line below.
Insertion
Insertion is at the lateral surface of the greater trochanter of the femur.
Activation Maneuver
Abduction of the thigh activates the muscle. The anterior fibers may also contribute to medial rotation of the thigh.
EMG Needle Insertion
Insert the needle 2-3 cm distal to the midpoint of the iliac crest.
Pitfalls
If the needle is inserted too anteriorly, it may be in the tensor fasciae latae, which is also supplied by the superior gluteal nerve and L4, L5 and S1 roots.
If the needle is inserted too posteriorly, it may be in the gluteus maximus, which is supplied by the inferior gluteal nerve and L5, S1, and S2 roots. The posterior third of the gluteus medius is covered by the gluteus maximus.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the superior gluteal nerve, sacral plexus, or L4, L5 S1, roots.
This is a good muscle to study for suspected L4 or L5 radiculopathy, because these roots primarily supply this muscle (Gray’s Anatomy, 1995).
Anatomical Illustrations
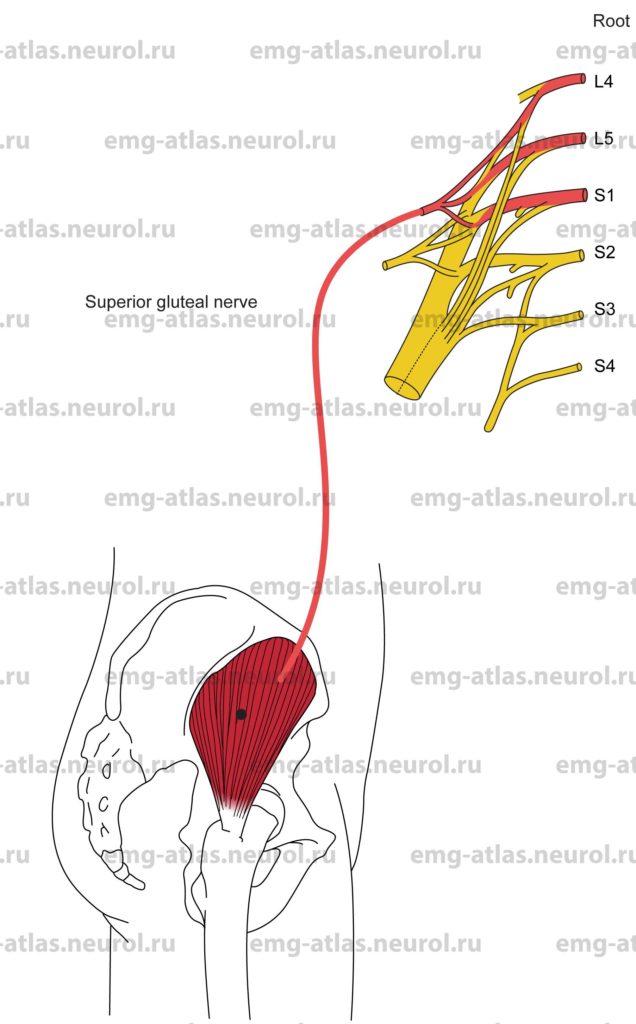
Gluteus Minimus
Innervation
Innervation is via the superior gluteal nerve, sacral plexus, and roots L4, L5 S1.
Origin
The gluteus minimus originates from the outer surface of the ilium between the anterior and inferior gluteal lines.
Insertion
Insertion is at the anterolateral surface of the greater trochanter of the femur.
Activation Maneuver
Abduction of the thigh activates the muscle. The anterior fibers may also contribute to medial rotation of the thigh.
EMG Needle Insertion
Insert the needle midway between the iliac crest and the greater trochanter of the femur.
Insert to the bone and withdraw slightly.
Pitfalls
There are no pitfalls. If the needle is inserted too superficially, it may be in the gluteus medius, which is also supplied by the superior gluteal nerve and L4, L5 S1, roots.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the superior gluteal nerve, sacral plexus, or L4, L5 S1, roots.
This is a good muscle to study for suspected L4 or L5 radiculopathy because these roots primarily supply this muscle (Gray’s Anatomy, 1995).
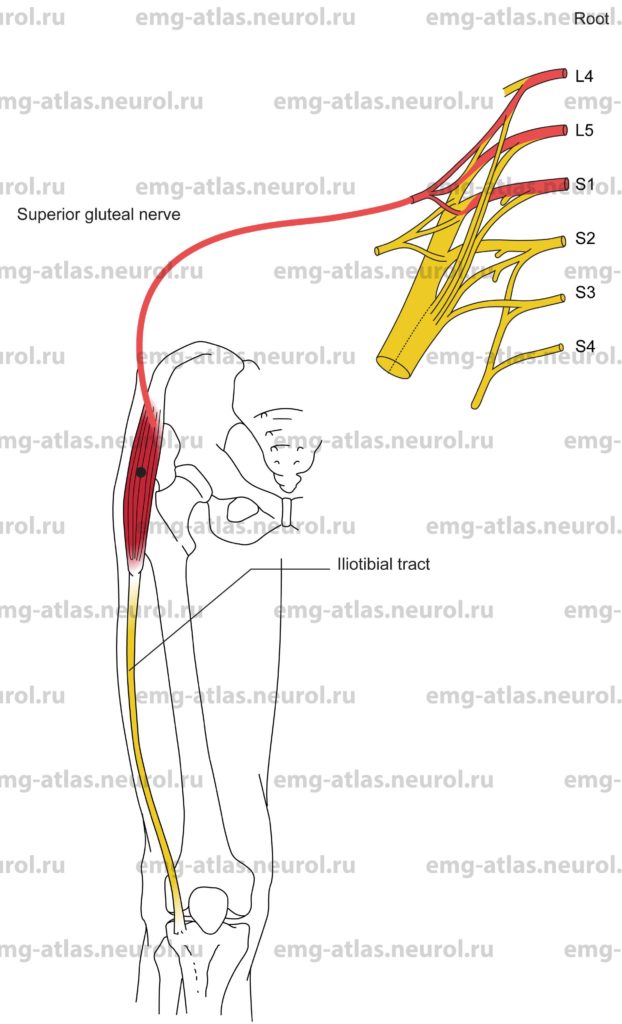
Anatomical Illustrations
Tensor Fasciae Latae
Innervation
Innervation is via the superior gluteal nerve, sacral plexus, and roots L4, L5 S1.
Origin
The tensor fasciae latae originates from the anterior superior iliac spine and the outer lip of the iliac crest
Insertion
Insertion is at the iliotibial tract of the fascia lata. The fascia lata is the deep of the thigh. It thickens over the flattened lateral surface of the thigh to form the iliotibial tract. The upper end of this tract splits into two layers, enclosing and anchoring the tensor fasciae latae below the greater trochanter of the femur.
Activation Maneuver
Medial rotation of the thigh activates the muscle. This muscle may also contribute to abduction of the thigh and, acting through the iliotibial tract, it may also extend the knee with lateral rotation of the leg (Gray’s Anatomy, 1995).
EMG Needle Insertion
Insert the needle midway between anterior superior iliac spine and the greater trochanter of the femur.
Pitfalls
If the needle is inserted too medially, it may be in the rectus femoris or sartorius, both muscles innervated by the femoral nerve and L2-L4 roots.
If the needle is inserted too laterally, it may be in the gluteus medius, which is also supplied by the superior gluteal nerve and L4, L5 and S1, roots.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the superior gluteal nerve, sacral plexus, or L4, L5 S1, roots.
This is a good muscle to study for suspected L4 or L5 radiculopathy because these roots primarily supply this muscle (Gray’s Anatomy, 1995).