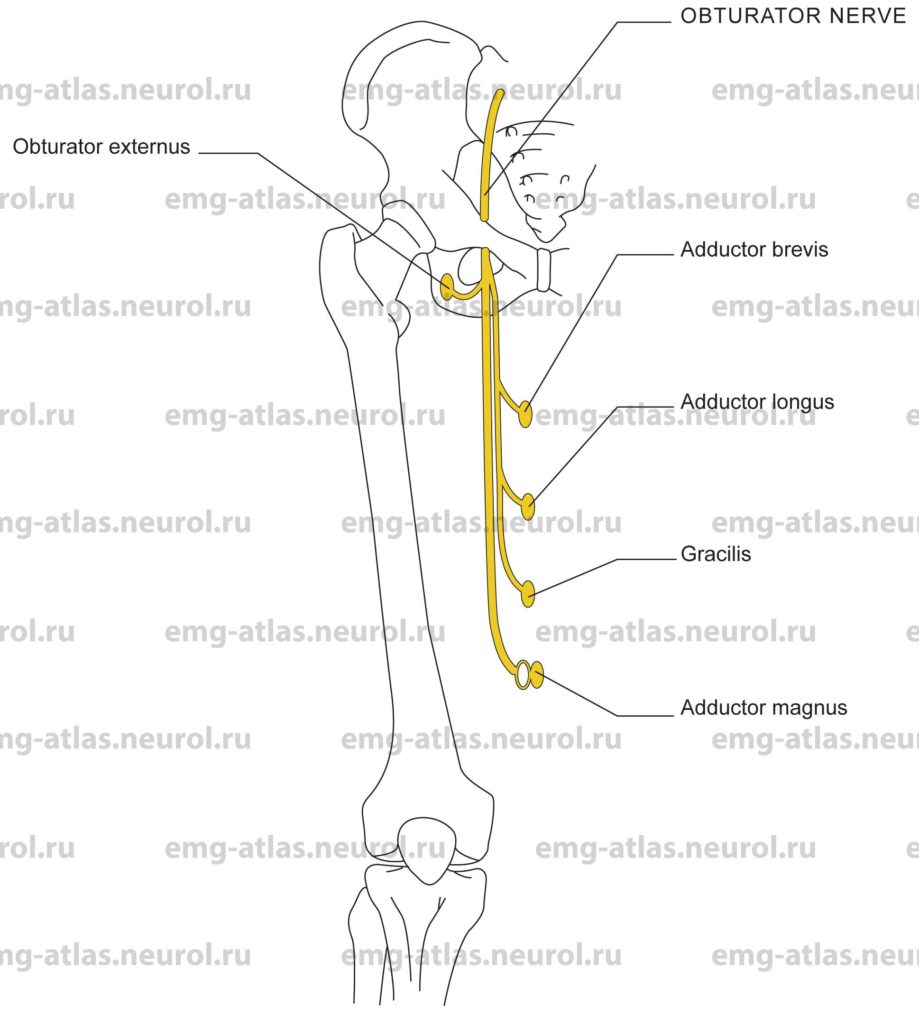
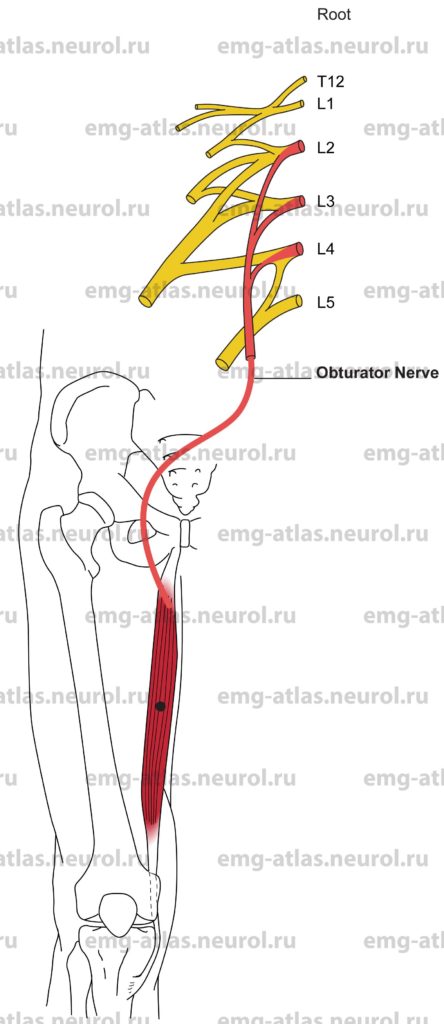
Diagram of the obturator nerve and the muscles that it supplies. NOTE: the white oval signifies that a muscle receives a part of its innervation from another peripheral nerve.
The obturator nerve arises from the anterior division of the second to fourth lumbar ventral rami. The contribution from the third or fourth ramus is the largest, and that from the second is often very small. The nerve descends within the substance of the psoas major, emerging from its medial border at the pelvic brim. It descends further along the ala of the sacrum to reach the lateral pelvic wall on the obturator internus muscle. It then sweeps forward within the pelvis to reach and pass through the obturator foramen to enter the thigh. Nearthe foramen it divides into anterior and posterior branches. The anterior branch supplies the adductor longus, adductor brevis, gracilis, and often the pectineus Gray’s Anatomy, 1995). At the lower border of the adductor longus, it communicates with the medial cutaneous and saphenous branches of the femoral nerve to supply the skin on the medial aspect of the thigh. The posterior branch supplies the obturator extermus and adductor magnus muscles. It usually sends an articular branch to the knee joint.
A small accessory obturator nerve may occasionally be present, arising from the anterior division of the third and fourth lumbar ventral rami to supply the pectineus and rarely the adductor longus muscles. Note the short muscles around the hip joint—obturator extermus, pectineus, quadratus femoris, gemellus superior, gemellus inferior, obturator internus, and piriformis—are largely innaccessible to direct observation. Because of the potential complications presented by their intimate relationship to important neurovascular structures, there is a total lack of EMG data from humans (Gray’s Anatomy, 1995).
Anatomical features of clinical importance relate to the posterior abdominal wall, where the obturator nerve may be involved together with the femoral nerve in retroperitoneal lesions. In the pelvis, compression of the nerve may occur against the lateral pelvic wall. Here the nerve may be in direct contact with the bone or separated from it by only a thin layer of muscle (Sunderland, 1968). It may be compressed by the fetal head during a difficult delivery or by a benign or malignant pelvic tumor or abscess. On the left side it may be involved by carcinoma of the sigmoid colon and on the right by an inflamed appendix. At the obturator foramen it is intimately related to the superior ramus of the pubis, and fractures of the bone may damage the nerve. Postsurgical obturator neuropathy has also been reported following positioning on the operating table in which the thigh is acutely flexed as in the lithotomy position. In these cases, nerve involvement is likely related to acute angulation where the nerve leaves the bony obturator foramen Sunderland, 1968). Neurectomy has been performed to relieve adductor spasms in disorders associated with upper motor neuron dysfunction.
Obturator Nerve Lesion
Etiology
Retroperitoneal lesions can cause an obturator nerve lesion. The obturator nerve may be involved together with the femoral nerve by hematoma, hemorrhage, tumor or abscess.
There are latrogenic causes, including neurectomy, repair of an obturator hernia, and postanesthesia compression due to acute angulation when the thigh is hyperflexed as in the lithotomy position.
Other causes include (1) compression of the nerve against the lateral pelvic wall by the fetal head or pelvic masses, (2) pelvic fractures, (3) penetrating injuries, and (4), neuralgic amyotrophy.
General Comments
It is common for an obturator nerve deficit to be accompanied by a femoral nerve deficit (Dawson et al., 1990). Lesions of the upper portion of the lumbar plexus usually affect both the obturator and femoral nerves because both arise from within the psoas muscle.
Most lesions that involve the obturator nerve are traumatic in origin.
In diabetic amyotrophy, proximal muscles are involved, including those innervated by the obturator nerve (Chokroverty and Sander, 1996).
Clinical Features
Paresis or paralysis of adductor muscles produces weakness or inability to adduct the thigh and leg.
Numbness, loss of sensation, or altered sensation in the medial aspect of the thigh can occur.
Loss or asymmetry of the adductor tendon reflex may be observed.
Electrodiagnostic Strategy
Perform EMG needle examination in thigh muscles innervated by the obturator nerve or its branches. In lesions associated with loss of motor fibers, EMG may show neurogenic changes (i.e., fibrillation potentials, polyphasic motor unit potentials, and neurogenic recruitment).
Perform EMG of quadriceps muscles, other proximal muscles (gluteal, hamstring), and paraspinal muscles to exclude plexus or root involvement.
Anatomical Illustrations
Adductor Longus
Innervation
Innervation is via the obturator nerve, anterior division of the lumbar plexus, and roots Lj, L3, L4.
Origin
The adductor longus originates at the front of the pubis, in the angle between the crest and the simphysis.
Insertion
Insertion is at the linea aspera in the middle third of the femur, between the vastus medialis and the other two adductors magnus and brevis).
Activation Maneuver
Adduction of the thigh activates the muscle.
EMG Needle Insertion
Insert the needle into the medial thigh 6-8 cm distal to the origin of the tendon near the pubic tubercle. The tendon can be easily palpated.
Pitfalls
If the needle is inserted too medially and anteriorly, it may be in the sartorius, which is supplied by the femoral nerve.
If the needle is inserted too laterally, it may be in pectineus, which is supplied by the femoral nerve (the pectineus may also receive a branch from obturator nerve).
If the needle is inserted too medially or posteriorly, it may be in the gracilis or the other two adductors, which are also supplied by the obturator nerve (the adductor magnus also receives a branch from the sciatic nerve).
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the obturator nerve, anterior division of the lumbar plexus, or L2, L3, L4 roots.
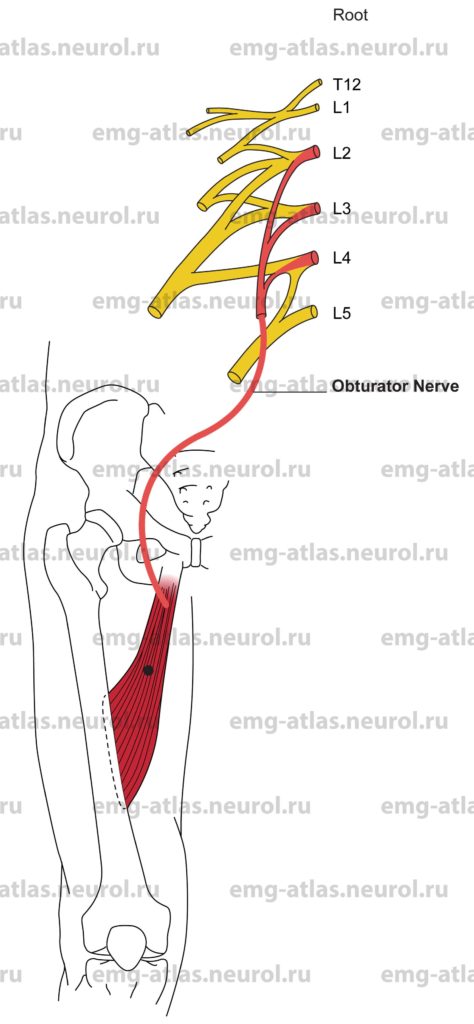
Anatomical Illustrations
Adductor Brevis
Innervation
Innervation is via the obturator nerve, anterior division of the lumbar plexus, and roots L2, L3, L4.
Origin
The adductor brevis originates at the inferior ramus of the pubis.
Insertion
Insertion is into the femur, along a line from the lesser trochanter to the linea aspera.
Activation Maneuver
Adduction of the thigh activates the muscle.
EMG Needle Insertion
Insert the needle into the medial thigh 5-7 cm distal to the origin of the tendon of adductor longus, to a depth of about 4 cm. The adductor brevis lies deep to the pectineus and adductor longus.
Pitfalls
If the needle is inserted too superficially, it may be in the pectineus or adductor longus, which are supplied by the femoral and obturator nerves, respectively. The pectineus may also receive a branch from the obturator nerve.
If the needle is inserted too medially, it may be in the gracilis, which is also supplied by the obturator nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the obturator nerve, anterior division of the lumbar plexus, or L2, L3, L4 roots.
Anatomical Illustrations
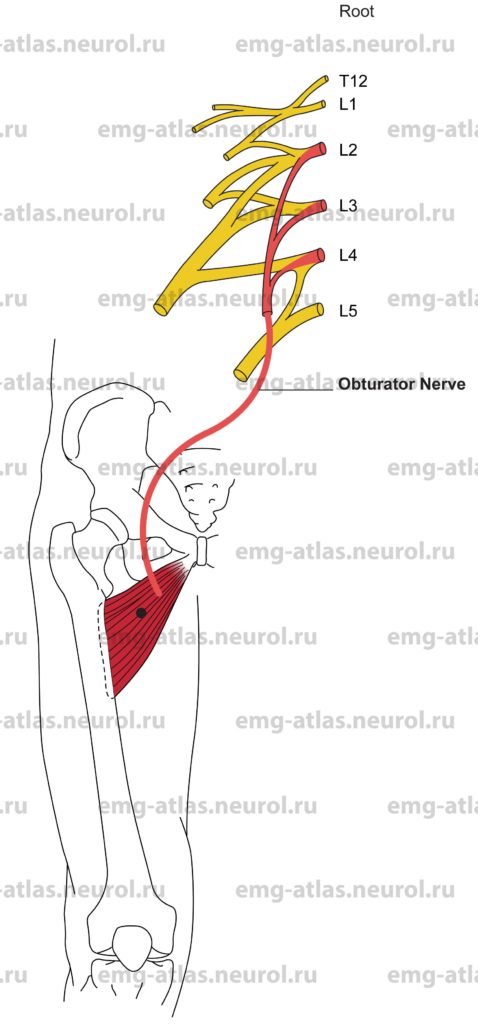
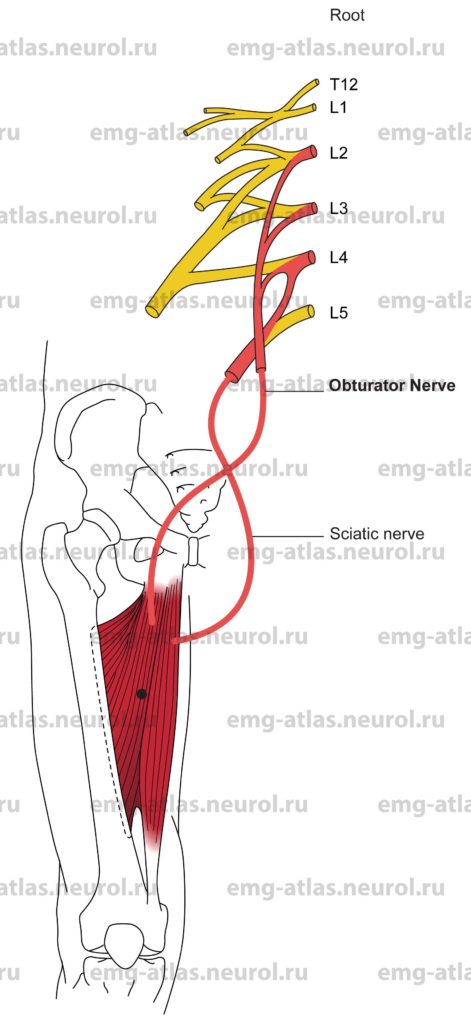
Adductor Magnus
Innervation
Innervation is via the obturator nerve, anterior division of the lumbar plexus, and roots L2, L3, L4.
Innervation is also via the sciatic nerve (tibial division), anterior division of the sacral plexus, and root L4.
Origin
The adductor magnus originates from a small part of the inferior ramus of the pubis, the conjoined ischial ramus, and inferolateral aspect of the ischial tuberosity.
Insertion
Insertion is into the gluteal tuberosity, linea aspera, medial supracondylar line, and adductor tubercle on the medial condyle of the femur. The sciatic nerve supplies the ischiocondylar fibers; the obturator nerve supplies the remaining fibers.
Activation Maneuver
Adduction of the thigh activates the muscle.
EMG Needle Insertion
Insert the needle into the medial thigh midway between the pubic tubercle and medial condyle of the femur.
Pitfalls
If the needle is inserted too laterally and anteriorly, it may be in the sartorius, which is supplied by the femoral nerve.
If the needle is inserted too posteriorly, it may be in the semitendinosus or semimembranosus, which are supplied by the sciatic nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the obturator nerve, anterior division of the lumbar plexus, or L2, L3, L4 roots. Neurogenic changes in ischiocondylar fibers may be seen with lesions of the sciatic nerve (tibial division), anterior division of the sacral plexus, or L4 root.
Morphologically, the ischiocondylar portion of the muscle may be considered to be a hamstring muscle, which explains its innervation from the sciatic nerve.
Anatomical Illustrations
Gracilis
Innervation
Innervation is via the obturator nerve, anterior division of the lumbar plexus, and L2, L3, L4 roots.
Origin
The gracilis originates at the inferior ramus of the pubis and adjoining part of the ischial ramus.
Insertion
Insertion is into the medial surface of the tibia, just below the medial condyle.
Activation Maneuver
Flexion and medial rotation of the leg activate the muscle. The gracilis may also adduct the thigh (Gray’s Anatomy, 1995).
EMG Needle Insertion
Insert the needle into the medial thigh midway between the pubic tubercle and medial condyle of the femur. The gracilis is the most superficial of the adductor group; it is thin and flat and may be missed by the needle.
Pitfalls
If the needle is inserted too anteriorly, it may be in the sartorius, which is supplied by the femoral nerve.
If the needle is inserted too posteriorly, it may be in the semimembranosus or semitendinosus, which are supplied by the sciatic nerve.
If the needle is inserted too deeply, it may be in the adductor magnus or the other two adductors, which are also supplied by the obturator nerve.
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the obturator nerve, anterior division of the lumbar plexus, or L2, L3, L4 roots.