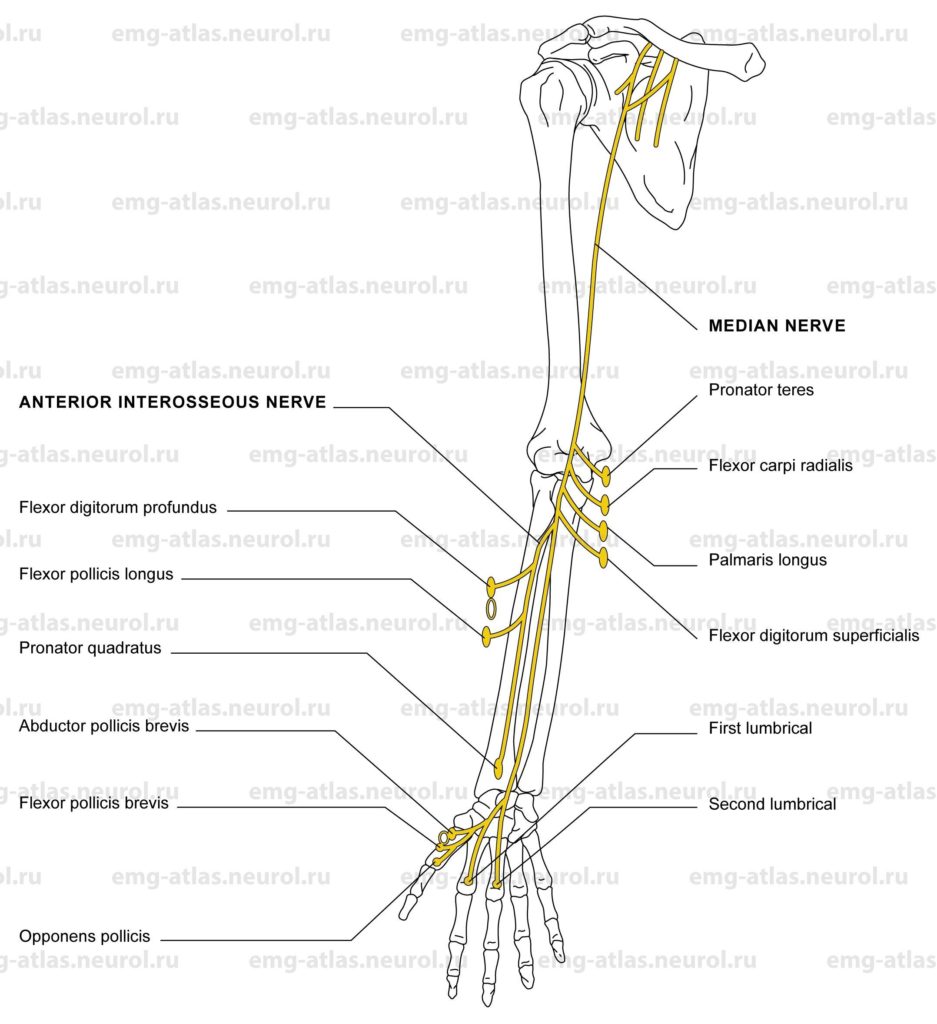
Diagram of the median nerve and the muscles that it supplies. Note: The white oval signifies that a muscle receives a part of its innervation from another peripheral nerve.
The median nerve is formed in the axilla from the medial and lateral cords of the brachial plexus. The lateral cord conveys fibers from the fifth, sixth, and seventh cervical spinal nerves, while the medial cord supplies fibers from the eighth cervical and first thoracic spinal nerves (Gray’s Anatomy, 1995). The median nerve innervates no muscles in the upper arm. In the cubital fossa, the nerve is accompanied by the brachial artery, which divides into radial and ulnar arteries at the neck of the radius. From this position, the nerve continues distally between the two heads of the pronator teres to reach the forearm proper. It supplies the pronator teres, flexor carpi radialis, palmaris longus, and flexor digitorum superficialis. It then gives rise to a pure motor branch, the anterior interosseous nerve, which innervates the flexor digitorum profundus to digits 2 and 3, flexor pollicis longus, and pronator quadratus. The nerve then descends the forearm and passes through the carpal tunnel as it enters the palm. It supplies the first and second lumbricals and gives off the recurrent thenar branch to the abductor pollicis brevis, flexor pollicis brevis (superficial head), and opponens pollicis. The median nerve also subserves sensation to the skin overlying the lateral aspect of the palm, dorsal surface of the distal phalanges, volar surface of the thumb, index and middle fingers, and half of the ring finger.
Although the median nerve, or its branches, may be affected by penetrating injuries at any level, there are certain sites where the nerve is prone to injury (Sunderland, 1968). In the upper arm, the nerve is closely bound to the axillary artery and then to the brachial artery as far as the cubital fossa. This close relationship explains why combined nerve-arterial injury is common in this region and why the nerve is subject to compression from aneurysms. In the lower arm, a spur of bone may rarely project from the anteromedial aspect of the supracondylar surface of the humerus and be joined to the medial epicondyle by a strong ligament (Struther’s ligament). This ligament may compress the median nerve proximal to the innervation to the pronator teres. In the pronator teres syndrome, the median nerve is injured in the upper forearm due to trauma, fracture, or, under exceptional circumstances, compression between the two heads of the pronator teres or a fibrous band as it emerges from this muscle. More distally in the forearm, the anterior interosseous branch may be injured by trauma or as a consequence of neuralgic amyotrophy. Entrapment of the anterior interosseous nerve may also result from fibrous bands or anomalous muscles (Wertsch, 1992). At the wrist, damage to the median nerve is commonly due to compression of the nerve in the carpal tunnel. This results in carpal tunnel syndrome, the most common entrapment neuropathy in humans.
Carpal Tunnel Syndrome
Etiology
Carpal tunnel syndrome is caused by compression of the nerve in the carpal tunnel.
General Comments
Carpal tunnel syndrome is the most common entrapment neuropathy. Women are affected more often than men.
Symptoms usually involve the dominant hand, with a higher incidence in persons who use their hands occupationally.
Predisposing conditions include obesity, pregnancy, polyneuropathy, diabetes, amyloidosis, acromegaly, rheumatoid arthritis, myxedema, and lupus erythematosus.
Clinical Features
Hand pain may be perceived more proximally in the forearm, arm, or shoulder, mimicking cervical radiculopathy.
Numbness usually involves the lateral four digits, but all digits may be affected or sensory loss may be confined to one digit.
Pain and paresthesia are aggravated by repetitive use of the hand.
Patients characteristically awaken at night with symptoms (nocturnal paresthesia).
In severe cases, there is weakness and atrophy of thenar muscles.
Onset is insidious in most cases.
Electrodiagnostic Strategy
Use nerve conduction studies to confirm a focal lesion of median sensory and motor fibers in the carpal tunnel. Many techniques have been developed for identifying conduction abnormalities within the carpal tunnel (Ross and Kimura, 1995).
Perform EMG needle examination in thenar muscles. In carpal tunnel syndrome associated with loss of motor fibers, EMG will show neurogenic changes (i.e., spontaneous activity, abnormal motor unit potentials, abnormal recruitment).
If EMG of thenar muscles is abnormal, study proximal median-innervated muscles to exclude median nerve lesion above the wrist. Also, study C8, T1 muscles innervated by ulnar or radial nerves to exclude C8, T1, radiculopathy.
If clinical symptoms or signs suggest cervical radiculopathy, study muscles supplied by C6 and C7 roots to exclude C6 or C7 radiculopathy. The differential diagnosis for carpal tunnel syndrome includes C6 and C7 radiculopathies due to overlap of dermatomes with median sensory distribution.
Anterior Interosseous Nerve Syndrome
Etiology
Neuralgic amyotrophy (idiopathic brachial plexopathy) may exclusively affect the anterior interosseous nerve (AIN).
Trauma, including stab wounds and gunshot wounds, can cause AIN syndrome.
Entrapment may rarely result from fibrous bands or anomalous muscles (Wertsch, 1992).
General Comments
The AIN is the largest branch of the median nerve.
It is a «pure» motor nerve because it lacks a cutaneous representation. However, sensory fibers from wrist and hand joints travel in the AIN.
The AIN innervates three muscles: flexor digitorum profundus (digits 2 and 3), flexor pollicis longus, and pronator quadratus.
Fifty percent of Martin-Gruber anastomoses arise from the AIN.
Clinical Features
A typical symptom is acute onset of thumb and index finger weakness.
Numbness and tingling do not occur.
A dull, aching pain may be present in the volar wrist or forearm.
The patient is unable to form an «O» with the thumb and index finger (due to weak flexion of terminal phalanges of the thumb and index finger).
Weakness in the pronator quadratus may be difficult to detect.
In a person with Martin-Gruber anastomosis and AIN syndrome, there may be additional weakness or atrophy of intrinsic hand muscles supplied by the crossing fibers (Wertsch, 1992).
The cutaneous sensory examination is normal.
Electrodiagnostic Strategy
Routine nerve conduction studies are normal.
Perform EMG needle examination in multiple muscles, including proximal and scapular muscles. EMG is crucial for identifying the possibility that AIN syndrome is a manifestation of neuralgic amyotrophy.
In AIN syndrome, EMG will show neurogenic changes (spontaneous activity, abnormal motor unit potentials, abnormal recruitment) in the flexor digitorum profundus to digits 2 and 3, flexor pollicis longus, and pronator quadratus.
In a person with Martin-Gruber anastomosis and AIN syndrome, EMG may show neurogenic changes in muscles supplied by the crossing fibers (usually dorsal interossei, adductor pollicis, or abductor digiti minimi).
Pronator Teres Syndrome
Etiology
Trauma, usually deep penetrating wounds, is causative.
Entrapment occurs between the two heads of the pronator teres or by a fibrous band connecting the pronator teres with the tendinous arch of the flexor digitorum superficial is.
General Comments
Some investigators have never encountered a true entrapment of the median nerve as it passes through the pronator teres; there is some doubt as to whether such an entrapment exists.
Clinical Features
Pain and tenderness occur over the pronator teres.
Numbness or tingling can occur in the median sensory distribution of the hand, including over the proximal palm and thenar eminence. (Note: The palmar cutaneous branch is spared in carpal tunnel syndrome because it passes superficial to the carpal tunnel. Sensory deficits in the palm and thenar eminence can help to differentiate pronator teres syndrome from carpal tunnel syndrome.)
In severe cases, there is weakness and atrophy of the median innervated muscles distal to the pronator teres.
Electrodiagnostic Strategy
Nerve conduction studies may show reduced conduction velocity or conduction block in the median nerve in the elbow to wrist segment.
EMG may show a neurogenic pattern in median-innervated muscles distal to the pronator teres.
Ligament of Struther’s Syndrome
Etiology
Entrapment is caused by Struther’s ligament, which is a fibrous band joining the supracondylar process (bony spur) on the anteromedial aspect of the lower humerus with the medial epicondyle of the humerus.
General Comments
A supracondylar process is present in only 0.3%-2.7% of humans (Pecina et al., 1997). When the supracondylar process is present, the median nerve and sometimes the brachial artery deviates medially to pass under Struther’s ligament
Clinical Features
Pain and paresthesia occur in the median sensory distribution of the hand, including the palm and thenar eminence (Note: The palmar cutaneous branch is spared in the carpal tunnel syndrome because it passes superficial to the carpal tunnel.)
In severe cases, there is weakness and atrophy of all median-innervated muscles, including the pronator teres. Weakness of pronation differentiates this condition from pronator teres syndrome.
Radiographic studies (plain films) show the supracondylar bony spur.
Electrodiagnostic Strategy
Nerve conduction studies may show reduced conduction velocity or conduction block in the median nerve in the upper arm to elbow segment.
Demonstrate neurogenic EMG in the median-innervated muscles, including the pronator teres.
Anatomical Illustrations
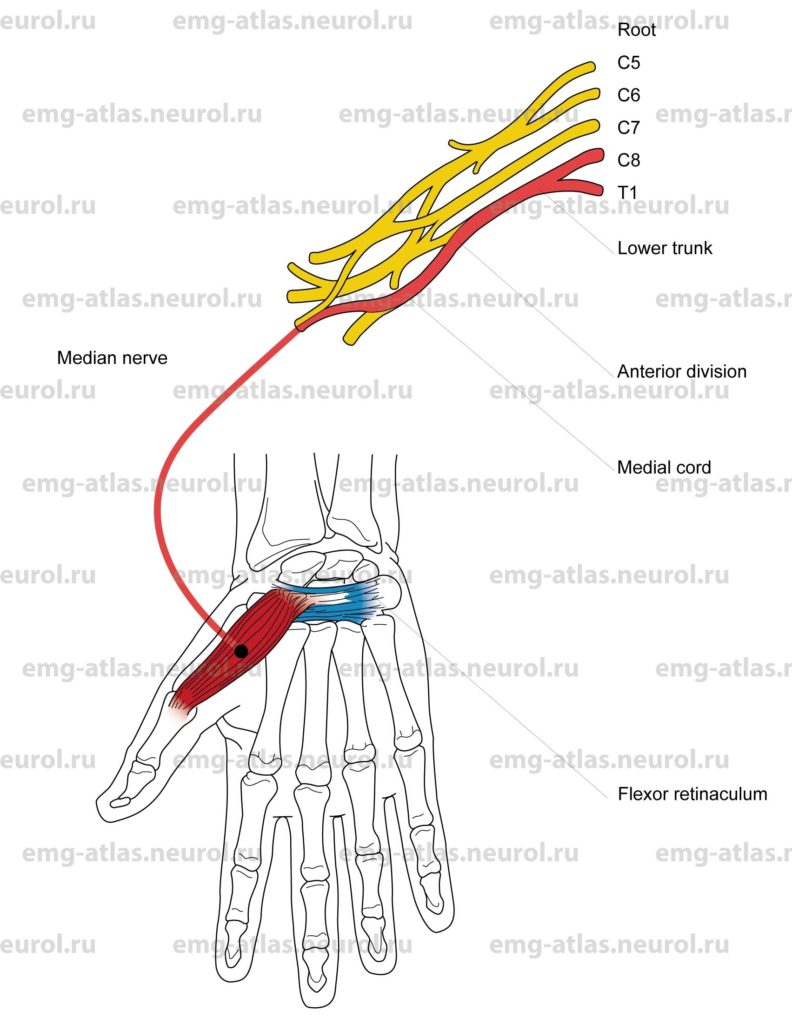
Abductor Pollicis Brevis
Innervation
Innervation is via the median nerve, medial cord, lower trunk, and roots C8, T1.
Origin
The muscle originates in the palmar retinaculum and the tubercle of the scaphoid and trapezium.
Insertion
The muscle is inserted at the base of the proximal phalanx of the thumb.
Activation Maneuver
Abduction of the thumb (movement of the thumb out of the plane of the palm) activates the muscle.
EMG Needle Insertion
Insert the needle obliquely near the muscle origin. Assess abnormal EMG activity by directing the needle distally along the muscle.
Pitfalls
If the needle is inserted too medially, it may penetrate the flexor pollicis brevis, which receives dual innervation from the median and ulnar nerves.
If the needle is inserted too deeply, it may penetrate the adductor pollicis, which receives innervation from the ulnar nerve.
Clinical Comments
Needle examination may show neurogenic changes with axonal loss lesions of the median nerve due to carpal tunnel syndrome, pronator teres syndrome, ligament of Struther’s syndrome, medial cord lesions, C8, T1, radiculopathy, Klumpke’s palsy (C8, T1, root avulsion), and anterior horn cell disease.
EMG will be normal in the anterior interosseous nerve syndrome.
Anatomical Illustrations
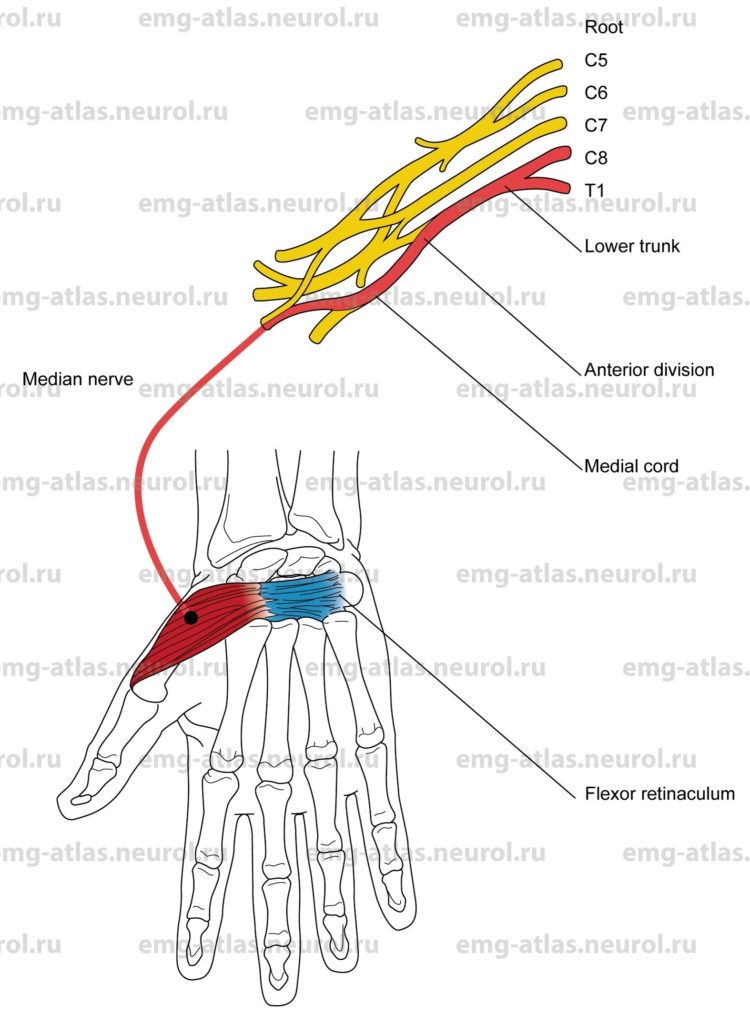
Opponens Pollicis
Innervation
Innervation is via the median nerve, medial cord, lower trunk, and roots C8, T1.
Origin
The muscle originates in the palmar retinaculum, and the tubercle of the trapezium.
Insertion
The muscle is inserted at the palmar surface of the first metacarpal bone.
Activation Maneuver
Opposition of the thumb to the little finger activates the muscle.
EMG Needle Insertion
Insert the needle obliquely at the midpoint of the first metacarpal shaft just lateral to the abductor pollicis brevis muscle.
Pitfalls
If the needle is inserted too medially, it will be in the abductor pollicis brevis, which still receives innervation from the median nerve.
If inserted even more medially, it may be in the flexor pollicis brevis, which receives dual innervation from the median and ulnar nerves. If the needle is inserted too deeply, it may penetrate the adductor pollicis, which receives innervation from the ulnar nerve.
Clinical Comments
EMG may show neurogenic changes in the carpal tunnel syndrome, pronator teres syndrome, ligament of Struther’s syndrome, medial cord lesions, C8, T, radiculopathy, Klumpke’s palsy (C8, T1, root avulsion), and anterior horn cell disease.
EMG will be normal in the anterior interosseous nerve syndrome.
Anatomical Illustrations
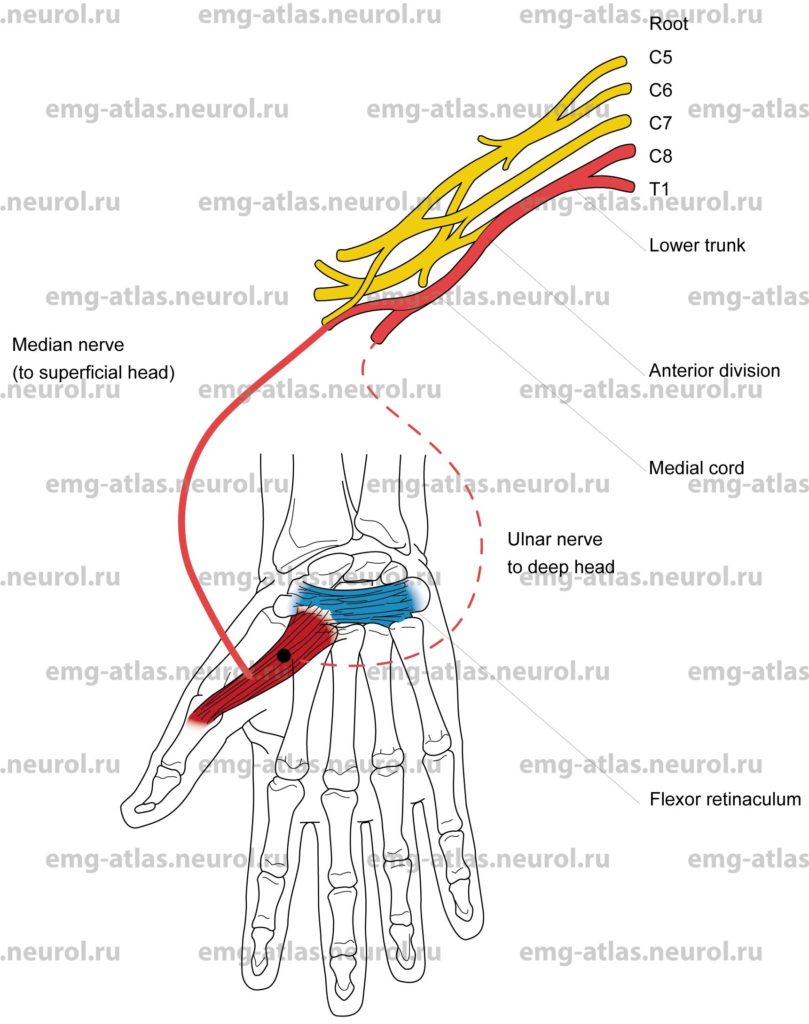
Flexor Pollicis Brevis
Innervation
Superficial head: Innervation is via the median nerve, medial cord, lower trunk, and roots C8, T1.
Deep head: Innervation is via the ulnar nerve, medial cord, lower trunk, and roots C8, T1.
Origin
The superficial head originates in the flexor retinaculum and trapezium.
The deep head originates in the ulnar aspect of the first metacarpal.
Insertion
The superficial head is inserted at the radial aspect of the base of the proximal phalanx of the thumb.
The deep head is inserted at the ulnar aspect of the base of the proximal phalanx of the thumb.
Activation Maneuver
Flexing of the metacarpophalangeal joint of the thumb activates the muscle.
EMG Needle Insertion
Superficial head: Insert the needle obliquely at a depth of 0.5-1 cm at the midpoint of a line drawn between the metacarpophalangeal joint and the pisiform.
Assess abnormal EMG activity by directing the needle distally along the muscle.
Deep head: The procedure is the same as that for the superficial head, but insert the needle to a depth of 1-2 cm.
Pitfalls
If the needle is inserted too deeply, it may penetrate the opponens pollicis, which is innervated by the median nerve; if inserted still deeper, it may be in the adductor pollicis, which receives innervation from the ulnar nerve.
If the needle is inserted too laterally, it will be in the abductor pollicis brevis, which receives innervation from the median nerve.
Clinical Comments
Testing of the flexor pollicis brevis is rarely of benefit in a routine EMG needle evaluation (in general, muscles that receive dual innervation should be avoided).
The superficial head will show neurogenic changes in lesions of the median nerve.
The deep head will show neurogenic changes in lesions of the ulnar nerve.
Both heads may show neurogenic changes in (C8, T1, radiculopathy, Klumpke’s palsy C8, T1, root avulsion), and anterior horn cell disease.
Anatomical Illustrations
1st, 2nd Lumbricals
Innervation
Innervation is via the median nerve, medial cord, lower trunk, and roots C8, T1.
Origin
The first and second lumbricals originate in the radial aspect of the tendon sheath of the flexor digitorum profundus.
Insertion
The muscles are inserted at the radial lateral band of the dorsal digital expansion.
Activation Maneuver
Extention of the finger at the proximal interphalangeal joint with the metacarpophalangeal joint extended and fixed activates the first and second lumbricals.
EMG Needle Insertion
Insert the needle just proximal to the metacarpophalangeal joint and radial to the flexor tendon.
Pitfalls
All muscles surrounding the first and second lumbricals receive innervation from the ulnar nerve. It is therefore easy to erroneously access ulnar intrinsic hand muscles.
Clinical Comments
Lumbrical examination causes pain. It is rarely of benefit in a routine EMG needle evaluation.
Needle examination will show neurogenic changes with axonal loss lesions of median nerve due to carpal tunnel syndrome, pronator teres syndrome, ligament of Struther’s syndrome, C8, T1, radiculopathy, Klumpke’s palsy (C8, T1, root avulsion), and anterior horn cell disease.
Anatomical Illustrations
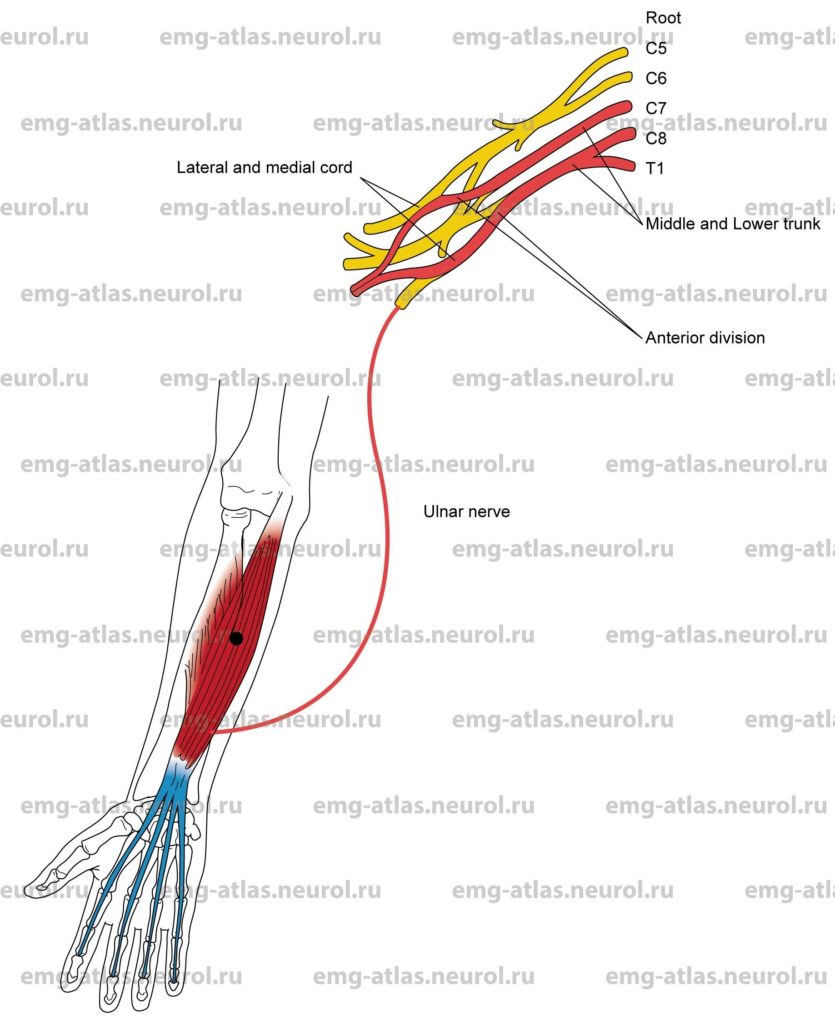
Pronator Quadratus
Innervation
Innervation is via the anterior interosseous branch, median nerve, lateral and medial cords, middle and lower trunks, and roots C7, C8, T1.
Origin
The pronator quadratus originates in the distal fourth of the volar surface of the ulna.
Insertion
The muscle is inserted at the distal fourth of the lateral border and the volar surface of the radius.
Activation Maneuver
Pronation of the forearm activates the muscle.
EMG Needle Insertion
Place the forearm in a neutral position to full supination (this opens up the area between the ulna and the radius). Insert the needle dorsally 2-3 cm proximal to the ulnar styloid just lateral (in the radial direction) to the ulna to a depth of 2-2.5 cm. Slant the needle slightly toward the shaft of the radius to penetrate the interosseous membrane.
Pitfalls
If the needle is inserted too deeply, it may penetrate the flexor digitorum superficialis, which receives innervation from the median nerve.
Clinical Comments
EMG needle examination will be normal in the carpal tunnel syndrome.
EMG may show neurogenic changes in lesions of the anterior interosseous nerve, producing axonal loss.
EMG may show neurogenic changes in more proximal lesions affecting median nerve fibers (pronator teres syndrome, ligament of Struther’s syndrome, C7, C8, T1, radiculopathy, root avulsion, and anterior horn cell disease).
Anatomical Illustrations
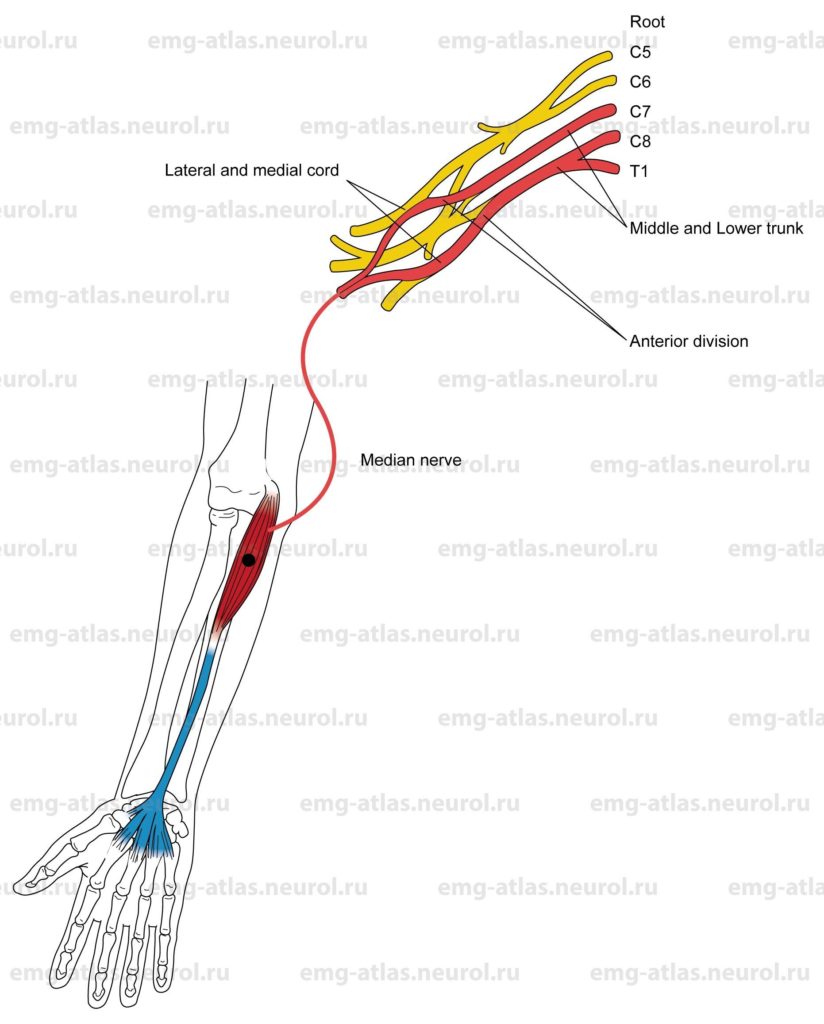
Flexor Pollicis Longus
Innervation
Innervation is via the anterior interosseous branch, median nerve, lateral and medial cords, middle and lower trunks, and roots C7, C8, T1.
Origin
The flexor pollicis longus originates in the volar surface of the radius.
Insertion
The muscle is inserted at the volar surface of the base of the distal phalanx of the thumb.
Activation Maneuver
Flexion of the distal phalanx of the thumb activates the flexor pollicis longus.
EMG Needle Insertion
Palpate the radial artery. Insert the needle 5-7 cm proximal and 1-1.5 cm lateral to the radial artery pulse.
Pitfalls
If the needle is inserted too superficially, it may lie in the flexor digitorum superficialis, which receives innervation from the median nerve.
If the needle is inserted too medially, the radial artery will lie in the path of the advancing needle.
Clinical Comments
EMG needle examination will be normal in the carpal tunnel syndrome.
EMG may show neurogenic changes in lesions of the anterior interosseous nerve, producing axonal loss.
EMG may show neurogenic changes in more proximal lesions affecting median nerve fibers (pronator teres syndrome, ligament of Struther’s syndrome, C7, C8, T1, radiculopathy, root avulsion, and anterior horn cell disease).
Anatomical Illustrations
Flexor Digitorum Profundus Digits 2 and 3
Innervation
Digits two and three: Innervation is via the anterior interosseous branch, median nerve, lateral and medial cords, middle and lower trunks, and roots C7, C8.
Digits four and five: Innervation is via the ulnar nerve, medial cord, lower trunk, and roots C8, T1.
Origin
The flexor digitorum profundus originates in the volar and medial surfaces of the ulna.
Insertion
The muscle is inserted at the volar surfaces of the bases of the distal phalanges of digits 2 through 5.
Activation Maneuver
Flexion of the distal phalanges of digits 2 through 5 activates the flexor digitorum profundus. EMG
Needle Insertion
Insert the needle 5-7 cm distal to the olecranon process and 1-1.5 cm medial to the shaft of the ulna. The ulnar innervated portion lies superficially at a depth of 1-2 cm; the median portion lies deep at a depth of 3-4 cm.
Pitfalls
If the needle is inserted too volarly (i.e., toward the palmar surface), it may lie in the flexor carpi ulnaris, which receives innervation from the ulnar nerve.
Clinical Comments
EMG of the deep portion may show neurogenic changes in the anterior interosseous nerve syndrome and in proximal lesions affecting median nerve fibers (pronator teres syndrome, ligament of Struther’s syndrome, C7, C8 radiculopathy, avulsion, and anterior horn cell disease).
EMG of the superficial portion may show neurogenic changes in axonal loss lesions of the ulnar nerve at the elbow (cubital tunnel or retrocondylar groove).
Anatomical Illustrations
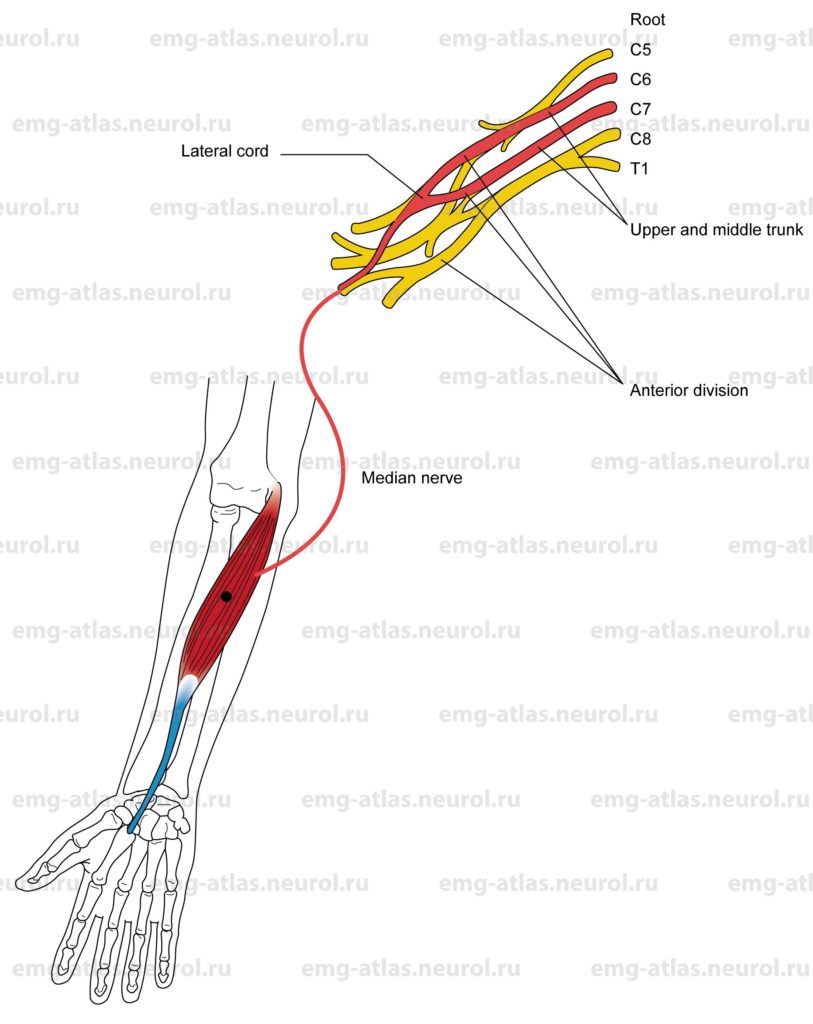
Flexor Digitorum Superficialis (sublimis)
Innervation
Innervation is via the median nerve, lateral and medial cords, middle and lower trunks, and roots C7, C8, T1.
Origin
The flexor digitorum superficialis (sublimis) originates in the Medial epicondyle of the humerus by the common tendon, coronoid process of ulna, and oblique line of the radius.
Insertion
Insertion is at the sides of the second phalanges of digits 2 through 5.
Activation Maneuver
Flexion of the digits at the proximal interphalangeal joint, with the proximal phalanx fixed and the distal interphalangeal joint in hyperextension, activates the muscle.
EMG Needle Insertion
Insert the needle into the volar surface of the forearm approximately 7-9 cm distal to the biceps tendon (midforearm) and 2-3 cm medial to the ventral midline.
Pitfalls
If the needle is inserted too laterally (radially), it may lie in the flexor carpi radialis, which also receives innervation from the median nerve.
If the needle is inserted too medially (ulnarly), it may be in the flexor carpi ulnaris, which receives innervation from the ulnar nerve.
If the needle is inserted too deeply, it may be in the flexor digitorum profundus (median innervated portion).
Clinical Comments
Needle examination may show neurogenic changes with axonal loss lesions of the median nerve due to pronator teres syndrome, ligament of Struther’s syndrome, brachial plexopathy, C7, C8, or T1, radiculopathies, and anterior horn cell disease.
Anatomical Illustrations
Palmaris Longus
Innervation
Innervation is via the median nerve, lateral and medial cords, middle and lower trunks, and roots C7, C8, T1.
Origin
The palmaris longus originates in the medial epicondyle of the humerus.
Insertion
Insertion is at the palmar aponeurosis.
Activation Maneuver
When the palm of the hand is cupped, the palmaris longus is activated. EMG Needle Insertion
Insert the needle into the volar surface of the forearm 6-8 cm distal to the medial epicondyle along a line directed toward the muscle tendon at the wrist.
Pitfalls
If the needle is inserted too laterally (radially), it may lie in the flexor carpi radialis, which receives innervation from the median nerve.
If the needle is inserted too medially (ulnarly), it may be in the flexor carpi ulnaris, which receives innervation from the ulnar nerve.
If the needle is inserted too deeply, it may be in the flexor digitorum superficialis median nerve innervation) or flexor digitorum profundus (median-innervated portion).
Clinical Comments
The palmaris longus is not routinely assessed. This muscle is the most variable muscle of the body (Bergman, et al., 1984). It is absent in 11% of humans (both arms in 8%; right arms, 4%; left arms, 5%).
Needle examination may show neurogenic changes with loss of axons in the median nerve due to pronator teres syndrome, ligament of Struther’s syndrome, brachial plexopathy, C7, C8, or T1, radiculopathies, and anterior horn cell disease.
Anatomical Illustrations
Flexor Carpi Radialis
Innervation
Innervation is via the median nerve, lateral cord, upper and middle trunks, and roots C6, C7.
Origin
The flexor carpi radialis originates in the medial epicondyle of the humerus.
Insertion
Insertion is at the volar surface of the base of the second metacarpal (a common variation is partial or total attachment to the trapezium).
EMG Needle Insertion
The needle is inserted into the volar surface of the forearm 7-9 cm distal to the medial epicondyle along a line directed toward the muscle tendon at the wrist.
Activation Maneuver
Flexion of the hand at the wrist with radial deviation activates the muscle. Hint: Avoid coactivation of the flexor digitorum superficialis or the pronator teres when performing the activation maneuver.
Pitfalls
If the needle is inserted too laterally (radially), it may be in the brachioradialis (radial nerve innervation); if it is inserted too lateral and proximal, it may be in the pronator teres (median nerve innervation).
If the needle is inserted too medially (ulnarly), it may be in the flexor digitorum superficialis or palmaris longus (median nerve innervation); if inserted too deeply, it will be in the flexor digitorum superficialis (median nerve innervation)
Clinical Comments
The flexor carpi radialis is routinely examined after carpal tunnel syndrome is diagnosed to exclude coexisting proximal median nerve injury (double lesion).
Needle examination may show neurogenic changes with loss of axons in the median nerve due to pronator teres syndrome, ligament of Struther’s syndrome, lateral cord lesion, C6, C7 radiculopathy, and anterior horn cell disease.
Anatomical Illustrations
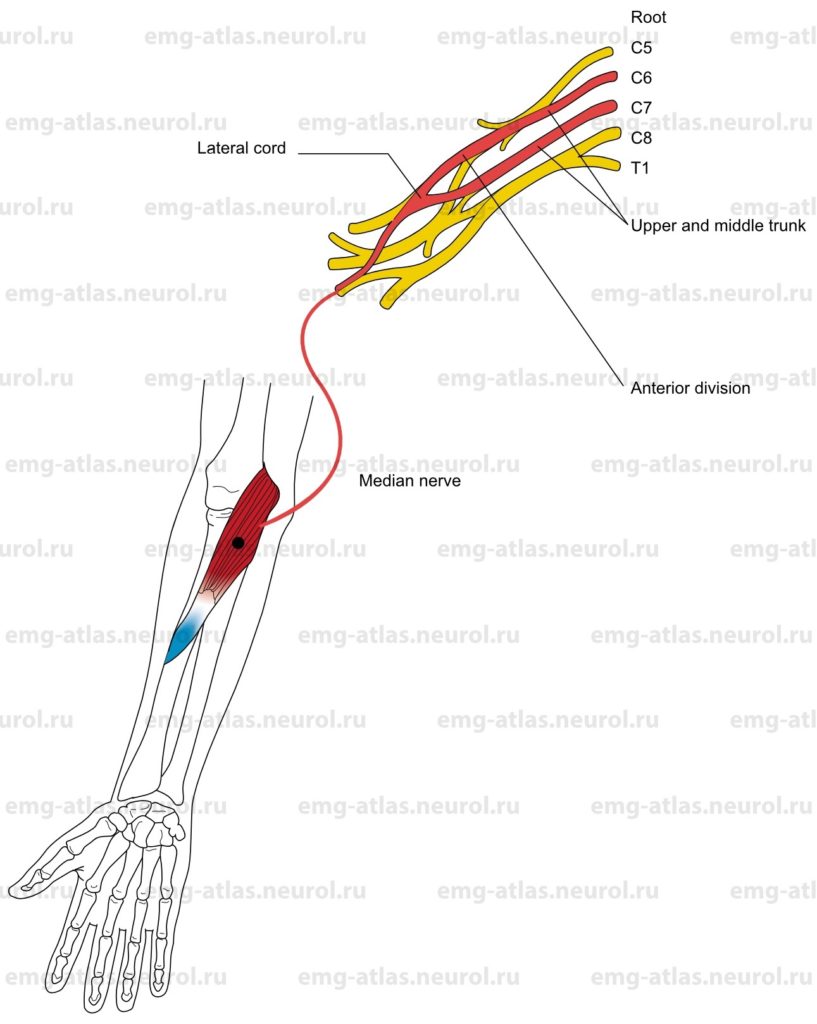
Pronator Teres
Innervation
Innervation is via the median nerve, lateral cord, upper and middle trunks, and roots C6, C7.
Origin
The pronator teres arises as two heads, one from the medial epicondyle of the humerus and the other from the coronoid process of the ulna.
Insertion
Insertion is at the lateral surface of the radius at the midshaft level. EMG Needle Insertion
Insert the needle 2-3 cm distal and 1 cm medial to the biceps tendon (the edge of the muscle can be palpated in this location).
Activation Maneuver
Pronation of the forearm activates the muscle. Hint: Avoid coactivation of the flexor carpi radialis when performing the activation maneuver.
Pitfalls
If the needle is inserted too laterally (radially), it may be in the brachioradialis, which is supplied by the radial nerve.
If the needle is inserted too medially (ulnarly) or too distally, it may be in the flexor carpi radialis, which is supplied by the median nerve.
If the needle is inserted too deeply, it will be in the flexor digitorum superficialis, which is supplied by the median nerve.
Clinical Comments
The pronator teres is the most proximal muscle innervated by the median nerve.
The median nerve enters the forearm between the two heads of this muscle. Entrapment produces the pronator teres syndrome.
EMG may show neurogenic changes with loss of axons in the median nerve due to ligament of Struther’s syndrome, lateral cord lesion, C6, C7 radiculopathy, and anterior horn cell disease.
EMG is usually normal in the pronator teres syndrome. Note: The muscle naming a syndrome is usually spared in that syndrome.