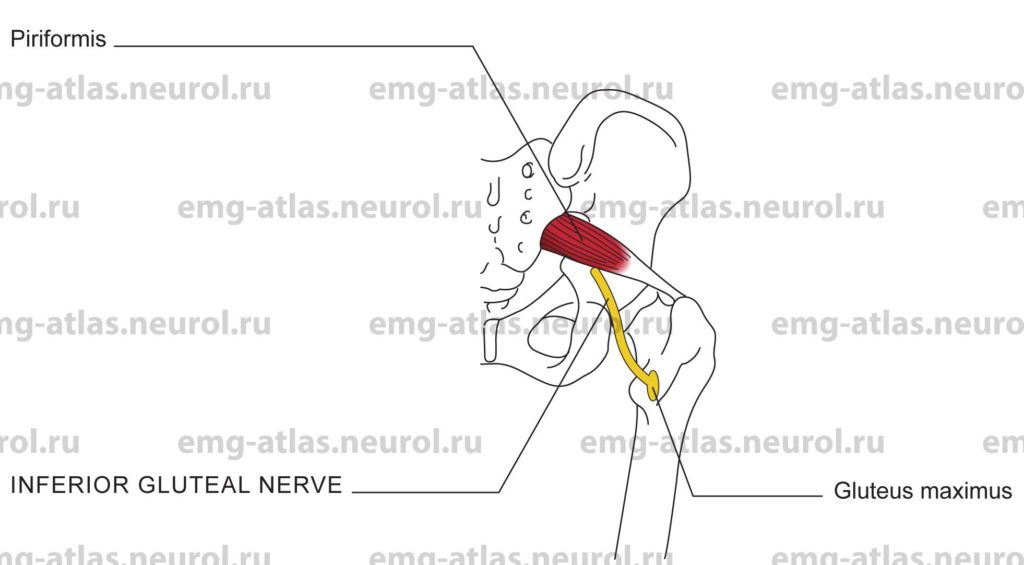
Diagram of the inferior gluteal nerve to the gluteus maximus (posterior view).
The inferior gluteal nerve arises from the posterior branches of the fifth lumbar and first and second sacral ventral rami (Gray’s Anatomy, 1995). It leaves the pelvis via the greater sciatic foramen below the piriformis muscle and divides into a number of branches that enter the deep surface of the gluteus maximus. The gluteus maximus is the largest and most superficial muscle of the gluteal region. It forms the familiar prominence of the buttock.
Anatomical Illustrations
Gluteus Maximus
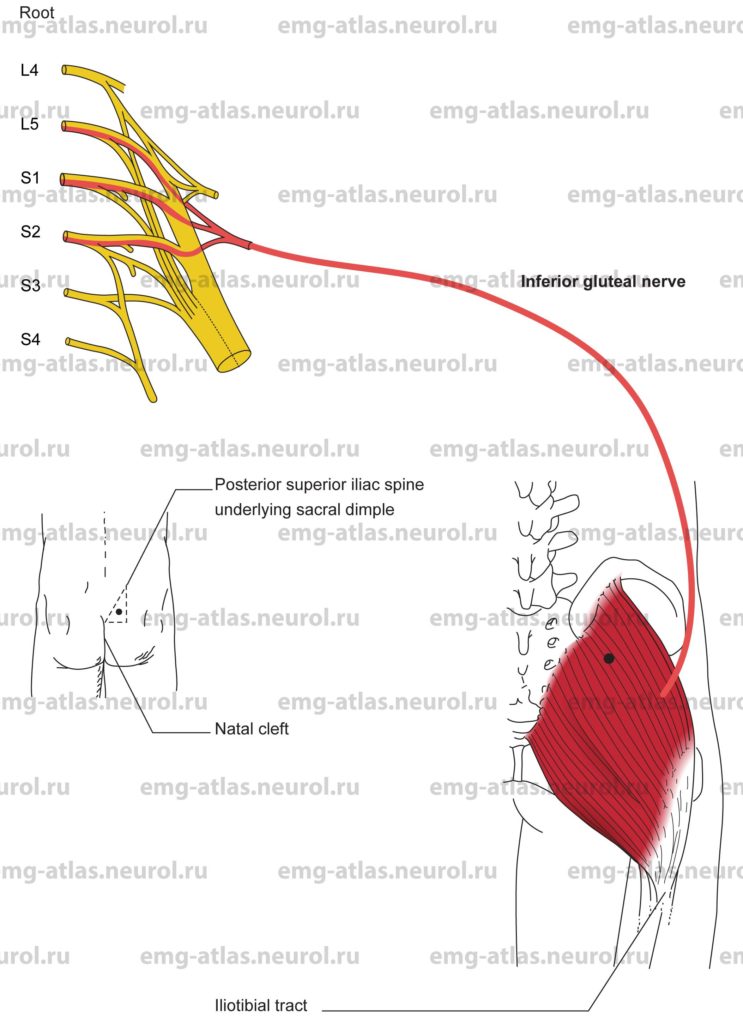
Innervation
Innervation is via the inferior gluteal nerve, sacral plexus, and roots L5, S1, S2.
Origin
The gluteus maximus originates from the posterior gluteal line of the ilium and the posterior iliac crest above the line, from the aponeurosis of the erector spinae, from the lower part of the sacrum and the side of the coccyx, and from the sacrotuberous ligament and the guteal fascia that covers the gluteus medius.
Insertion
Insertion is at the iliotibial tract of the fascia lata and the gluteal tuberosity of the femur. The fascia lata is the deep fascia of the thigh. It thickens over the flattened lateral surface of the thigh to form the iliotibial tract.
Activation Maneuver
Extension of the thigh with the knee flexed activates the muscle. The patient can also be asked to contract or tighten the buttock muscles. The gluteus maximus contributes to external rotation of the thigh and, acting through the iliotibial tract, stabilizes the femur on the tibia (Gray’s Anatomy, 1995).
EMG Needle Insertion
Insert the needle inside an imaginary right triangle with the hypotenuse of the triangle formed by a line connecting the posterior superior iliac spine (underlying the sacral dimple) and the commencement of the natal cleft (corresponding to the third sacral spine). This will avoid the sciatic nerve, which exits the pelvis more laterally and inferiorly below the piriformis and descends between the greater trochanter and ischial tuberosity.
Pitfalls
If the needle is inserted too laterally and inferiorly, it may encounter the sciatic nerve. Sciatic neuropathy from direct needle injury or associated hematoma is a potential complication (Sunderland, 1968; Villarejo and Pascual, 1993). It is therefore prudent to avoid needle examination of that portion of gluteus maximus that overlies the sciatic nerve. Avoid the region below the piriformis and between the greater trochanter and ischial tuberosity. Muscles in this region intimately associated with the sciatic nerve include the gemellus superior and inferior, obturator internus, and quadratus femoris.)
Clinical Comments
Neurogenic changes on needle examination may be seen with lesions of the inferior gluteal nerve, sacral plexus, or L5, S1, S2 roots.
This is a good muscle to study for suspected L5 or S1 radiculopathy because these roots primarily supply this muscle (Gray’s Anatomy, 1995).